Bioequivalence Waivers: When the FDA Allows Generic Drugs Without Human Trials
Most people assume that before a generic drug hits the shelf, it must be tested in people. That’s not always true. The FDA lets companies skip human trials entirely - if the science justifies it. This is called a bioequivalence waiver, or biowaiver. It’s not a loophole. It’s a scientifically proven shortcut that saves time, money, and avoids unnecessary testing on volunteers.
Why the FDA Allows Biowaivers
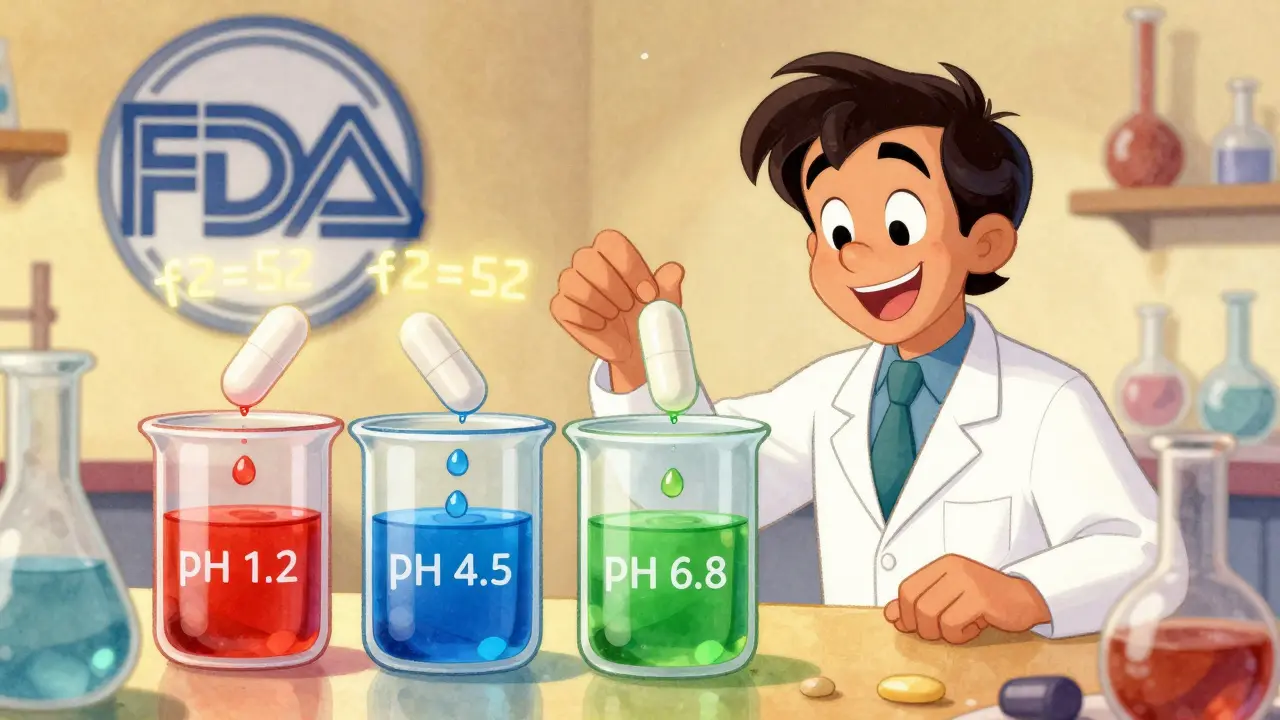
The FDA doesn’t want to run blood tests on healthy volunteers unless it’s absolutely necessary. If a drug’s behavior in the body can be predicted just by testing how it dissolves in a lab, then why put people through it? That’s the core idea behind biowaivers. For certain types of drugs, especially simple immediate-release pills, dissolution testing in the lab is more reliable than measuring drug levels in blood. The science behind this comes from the Biopharmaceutics Classification System (BCS). It sorts drugs into four classes based on how well they dissolve in water and how easily they cross the gut wall. Only two classes qualify for biowaivers: Class I and Class III. Class I drugs are the easiest. They dissolve quickly and are absorbed completely. Think of drugs like metformin, atenolol, or ranitidine. If two versions of a Class I drug dissolve at the same rate in the lab - under pH conditions that mimic the stomach and intestines - the FDA accepts that they’ll behave the same in the body. No blood draws needed. Class III drugs are trickier. They dissolve well but don’t cross the gut wall easily. For these, the FDA requires more proof: identical ingredients, same amounts of each excipient, and evidence that absorption doesn’t change depending on where in the gut the drug is released. Fewer drugs fall into this category, and approvals are harder to get.How a Biowaiver Works in Practice
To get a biowaiver, a company must prove two things: the drug fits the BCS criteria, and its dissolution profile matches the reference product. The FDA requires dissolution tests using at least 12 tablets or capsules per batch. Testing happens in three different pH solutions: stomach acid (pH 1.2), the upper intestine (pH 4.5), and the lower intestine (pH 6.8). Samples are taken every 10 to 60 minutes to build a full dissolution curve. The key number? The f2 similarity factor. If the test product’s dissolution curve matches the brand-name drug’s curve within an f2 score of 50 or higher, the FDA considers them equivalent. That’s not guesswork - it’s a math-based comparison that shows how closely the two products release their drug over time. This isn’t just paperwork. It takes months of method development. Formulation scientists spend time tweaking the dissolution test to make sure it can detect even tiny differences between products. If the method isn’t sensitive enough, the FDA rejects the waiver. In fact, 35% of failed biowaiver applications were turned down because the dissolution method couldn’t tell the difference between similar-looking pills.Cost and Time Savings Are Massive
A traditional bioequivalence study - where 24 to 36 volunteers take both the generic and brand-name drug, then have their blood drawn multiple times - costs between $250,000 and $500,000. It takes six to twelve months to complete. A biowaiver? It can be done in two to three months for under $50,000. That’s why generic drug makers use biowaivers aggressively. In 2022, nearly 18% of all ANDA applications for solid oral drugs included a biowaiver request - up from 12% in 2018. Companies like Teva and Mylan use biowaivers in 25-30% of their pipelines. Smaller firms use them less often, mostly because they lack the in-house expertise to design the right dissolution tests. One formulation scientist reported saving $4.2 million over three years by getting 12 biowaivers approved. Each approval shaved off 8 to 10 months from the timeline. That means generic versions hit the market faster, lowering prices sooner.
What Doesn’t Qualify
Biowaivers are not a free pass for all drugs. The FDA explicitly excludes:- Modified-release products (extended-release, delayed-release)
- Narrow therapeutic index drugs (like warfarin, lithium, or digoxin), except for a few antiepileptics
- Drugs with solubility or permeability issues (BCS Class II and IV)
- Locally acting drugs (like inhalers or topical creams)
Industry Gaps and FDA Challenges
Even when companies follow the rules, approval isn’t guaranteed. A regulatory affairs specialist noted that three out of five Class III biowaiver submissions were rejected - even when they met all technical criteria. Why? Inconsistent interpretation across FDA review divisions. A 2022 PhRMA survey found that 42% of companies experienced uneven standards. One team might approve a waiver based on f2 = 52; another might demand f2 = 60. There’s no official threshold beyond “≥50,” so reviewers sometimes apply their own interpretations. The FDA is trying to fix this. Their 2023-2027 strategic plan aims to expand biowaiver opportunities by 25% through better models that link lab data to real-world performance. They’ve also invested $15 million annually in GDUFA to improve dissolution testing methods.
What’s Next for Biowaivers
The future is expanding - slowly. The FDA’s 2022 draft guidance opened the door for more Class III drugs, provided extra data is submitted. ICH M9, an international standard adopted in 2021, helps harmonize biowaiver rules across the U.S., EU, and Japan. Analysts predict that by 2027, biowaivers could be used in 25-30% of all generic drug applications. That means more affordable medications reaching patients faster. But the real challenge isn’t science - it’s consistency. Until every FDA reviewer applies the same standards, companies will keep facing unpredictable delays.Bottom Line
Bioequivalence waivers aren’t about cutting corners. They’re about using smarter science. For simple, well-understood drugs, dissolution testing is more accurate than human trials. The FDA knows this. That’s why they’ve built a framework that lets companies skip the blood draws - if they can prove it’s safe to do so. For patients, this means faster access to cheaper generics. For manufacturers, it means lower costs and quicker launches. For regulators, it means fewer volunteers exposed to unnecessary testing. Everyone wins - when the science is solid.What drugs qualify for an FDA bioequivalence waiver?
Only immediate-release solid oral dosage forms that meet BCS Class I (high solubility, high permeability) or Class III (high solubility, low permeability) criteria. Examples include metformin, atenolol, and ranitidine. Modified-release, narrow therapeutic index, and poorly soluble drugs (BCS Class II and IV) do not qualify.
Do I need human volunteers for a biowaiver?
No. A bioequivalence waiver means the FDA waives the requirement for in vivo human studies. Approval is based entirely on in vitro dissolution testing under controlled lab conditions.
What is the f2 similarity factor and why does it matter?
The f2 factor is a statistical measure that compares the dissolution profiles of two drug products. An f2 score of 50 or higher means the test product releases its active ingredient similarly to the reference product. The FDA requires this to approve a biowaiver - it’s the main proof that the two drugs will behave the same in the body.
Why do some biowaiver applications get rejected?
The most common reason is inadequate dissolution method discrimination - the test can’t detect differences between formulations. Other reasons include incorrect pH conditions, insufficient sampling points, or failure to prove identical excipients for Class III drugs. About 35% of rejections are due to poor method validation.
Can biowaivers be used for brand-name drugs too?
Yes. Biowaivers apply to both generic and brand-name drug applications. If a company changes the formulation of a brand-name drug (e.g., switching manufacturers or adding a new excipient), they can request a biowaiver instead of running a new human study - if the BCS criteria are met.
How long does a biowaiver application take to approve?
The review time is typically 10-12 months, similar to a full ANDA. But because no clinical trial is needed, the overall development timeline is shortened by 8-10 months compared to traditional bioequivalence studies. Early consultation with the FDA through the Pre-ANDA program increases approval chances by 22%.
Are biowaivers accepted outside the U.S.?
Yes. The International Council for Harmonisation (ICH) adopted guideline M9 in 2021, which standardizes BCS-based biowaivers across the U.S., EU, Japan, Canada, and other member countries. This means a biowaiver approved in the U.S. is often accepted internationally, reducing redundant testing.

This is just the FDA letting Big Pharma off the hook under the guise of 'science.' They don't want to test drugs on people because it's expensive and messy - so they let companies fudge dissolution curves and call it 'equivalent.' I've seen labs where the pH buffers were off by 0.3 and nobody noticed. You think metformin behaves the same in your gut as in a beaker? Please. They're gambling with lives and calling it efficiency.
Oh please, Charles, you sound like a 19th-century physician screaming about germ theory. The BCS isn't some corporate fantasy - it's peer-reviewed, validated, and adopted globally. The f2 factor has been statistically proven across thousands of formulations. If you're too lazy to understand dissolution kinetics, don't blame the system for being too smart for you.
It's fascinating how we've shifted from 'trust the doctor' to 'trust the dissolution curve.' We're outsourcing biological prediction to math and machinery. But what does that say about our relationship with medicine? Are we now treating the body like a chemical reactor? I'm not saying it's wrong - just deeply ironic that we've become so confident in in vitro models that we're willing to skip the living system entirely.
Look, I’ve worked in generic pharma for 18 years. I’ve seen biowaivers save lives - not because they're perfect, but because they get life-saving meds to people who can’t afford the brand. I remember a guy in rural Alabama getting his metformin for $4 instead of $400 because of a biowaiver. That’s not corporate greed - that’s public health winning. Yeah, the method isn’t flawless, but it’s better than making people wait two extra years while some lab runs 36 blood draws on college kids who need rent money.
And yeah, some reviewers are inconsistent. But that’s bureaucracy, not science. Fix the process, don’t trash the principle.
Whatever. Just give me the cheap pills. Don't care how they got approved.
I’ve spent years in labs watching these dissolution tests. It’s not magic - it’s meticulous. We tweak buffers, calibrate probes, run 12 tablets per batch, repeat across pH 1.2, 4.5, and 6.8 - sometimes for months just to get the method sensitive enough. And when the f2 hits 52? That’s not luck. That’s science with sweat. The real tragedy isn’t the waiver - it’s that small companies can’t afford to play this game. The system rewards deep pockets, not just good science.
So the FDA lets generics skip human trials if the pill dissolves right in a beaker. Sounds crazy until you realize we've been doing this for 20 years and no one's dropped dead from a bad generic. The system works. People who complain about it are either scared of change or got burned by a bad batch - and that’s a manufacturing issue, not a regulatory one.
It is deeply concerning that the United States Food and Drug Administration has permitted the circumvention of in vivo bioequivalence testing for certain pharmaceutical agents, particularly when international regulatory bodies maintain more stringent protocols. This represents a dangerous erosion of pharmacovigilance standards and invites potential public health risks. The American public deserves better than this deregulatory drift.
We think we’ve mastered biology by reducing it to curves and numbers. But the body isn’t a beaker. It’s a symphony - gut flora, food interactions, genetic variability, circadian rhythms. We’re not just skipping human trials - we’re pretending the human isn’t there. And that’s not science. That’s arrogance dressed in lab coats.
Biowaivers are scientifically valid and cost-effective. The FDA's framework is well-established and internationally recognized. For Class I and III drugs, dissolution testing is sufficient. This approach aligns with global standards and improves patient access.
Okay but like… imagine if your birth control pill dissolved 10% slower and you got pregnant because some FDA reviewer was like ‘eh, f2=51 is close enough’ 😭 and then you’re like ‘wait but I read the label’ and your ex is like ‘so… you’re telling me the generic was the problem??’ 🤡 I’m not saying it’s wrong, I’m saying I’d rather pay $50 for the brand and sleep at night. Also why does the FDA have 3 different teams giving different answers? That’s not science, that’s chaos with a clipboard.
This is actually beautiful. Science evolving to protect people AND the planet - fewer volunteers, less waste, faster access. 💚 The real enemy isn’t the waiver - it’s when big companies hoard the tools to prove it. Let’s fund small labs, train more people in dissolution science, and make this fair for everyone. We can fix the inconsistency - but don’t throw out the baby with the bathwater. 🙏
The philosophical underpinning of the biowaiver rests upon a reductionist epistemology - the belief that measurable physicochemical properties can fully represent complex biological outcomes. While empirically successful in many cases, this paradigm risks obscuring the ontological distinction between the chemical entity and its lived physiological manifestation. The dissolution curve, however precise, remains a proxy - never the phenomenon itself. We must remain vigilant against conflating measurement with reality.