Diabetic Nephropathy: How ACE Inhibitors, ARBs, and Protein Control Protect Your Kidneys
When you have diabetes, your kidneys are under constant stress. Over time, high blood sugar damages the tiny filters in your kidneys, causing them to leak protein into your urine. This isn’t just a lab result-it’s the early warning sign of diabetic nephropathy, the leading cause of kidney failure in people with diabetes. Left unchecked, it can lead to dialysis or transplant. But here’s the good news: two classes of blood pressure medicines-ACE inhibitors and ARBs-have been proven to slow or even stop this damage. And the key isn’t just taking them. It’s taking them at the right dose.
What Diabetic Nephropathy Really Means
Diabetic nephropathy isn’t just "kidney problems" from diabetes. It’s a specific pattern of damage: persistent albuminuria (more than 30 mg of protein in your urine per day) confirmed over three months or more. You might not feel sick. No swelling, no pain. But your kidneys are quietly failing. By the time symptoms show up, the damage is often advanced. That’s why screening matters. If you have type 1 or type 2 diabetes, you should get a urine test for albumin at least once a year.
This condition doesn’t happen in isolation. People with diabetic nephropathy are also at much higher risk for heart attacks and strokes. The same damaged blood vessels that leak protein in the kidneys are also clogging arteries in the heart and brain. That’s why treatment isn’t just about protecting your kidneys-it’s about protecting your whole body.
Why ACE Inhibitors and ARBs Are the First Line of Defense
For over 20 years, ACE inhibitors and ARBs have been the go-to treatment for diabetic nephropathy. Why? Because they do two things at once: lower blood pressure and directly protect the kidneys.
These drugs block the renin-angiotensin-aldosterone system (RAAS), a hormone pathway that tightens blood vessels and increases pressure inside the kidney’s filtering units. When that pressure drops, the filters stop leaking protein. Less protein in the urine means slower kidney damage. Clinical trials like RENAAL and IDNT showed that ARBs like losartan and irbesartan cut the risk of kidney failure by up to 30% in patients with heavy proteinuria.
ACE inhibitors like captopril, ramipril, and benazepril work the same way. In fact, captopril is the only ACE inhibitor with an FDA-approved label specifically for diabetic nephropathy. But don’t let that fool you-other ACE inhibitors are just as effective when used at the right dose. The brand doesn’t matter as much as the dose.
Protein Control Isn’t Optional-It’s the Goal
Doctors don’t just prescribe ACE inhibitors or ARBs to lower blood pressure. They prescribe them to reduce protein in the urine. That’s the real target. If your urine test shows more than 300 mg of albumin per gram of creatinine (called severely increased albuminuria), guidelines say you should be on one of these drugs at the highest tolerated dose.
Many patients get started on low doses-10 mg of lisinopril, 50 mg of losartan-and stay there. But that’s not enough. The studies that proved these drugs work used doses at the top end of the approved range: 100 mg of losartan, 20 mg of ramipril, 25 mg of captopril three times a day. If you’re not hitting those levels, you’re not getting the full kidney protection.
Here’s what you need to know: if your creatinine rises by less than 30% after starting the drug, don’t stop it. That’s normal. It means your kidneys are adjusting to lower pressure. Stopping the medicine because of this small rise is one of the most common mistakes in diabetes care. It leaves your kidneys vulnerable.

When Not to Use These Drugs
ACE inhibitors and ARBs aren’t for everyone. If you’re not hypertensive and your urine protein is normal (under 30 mg/day), these drugs won’t help prevent kidney disease. Studies show no benefit in people with type 1 diabetes who have normal blood pressure and no protein leakage. The NIH and ADA both say: don’t use them for primary prevention in this group.
They’re also risky if you’re pregnant. These drugs can cause serious birth defects. If you’re planning a pregnancy or think you might be pregnant, talk to your doctor right away. There are safer alternatives.
And never combine an ACE inhibitor with an ARB. The VA NEPHRON-D, ONTARGET, and ALTITUDE trials all showed the same thing: doubling up doesn’t help. It just raises your risk of dangerous side effects-high potassium levels (hyperkalemia) and sudden kidney failure. Even adding a direct renin inhibitor like aliskiren on top of these drugs is not recommended. More isn’t better here.
What About Other Medications?
Diuretics, calcium channel blockers, and beta blockers are still important-but not as first choices. Use them to help control blood pressure once you’re already on an ACE inhibitor or ARB. They don’t offer the same kidney protection. If you can’t tolerate an ACE inhibitor or ARB (maybe you get a persistent cough from an ACE inhibitor), then a calcium channel blocker like amlodipine is the next best option.
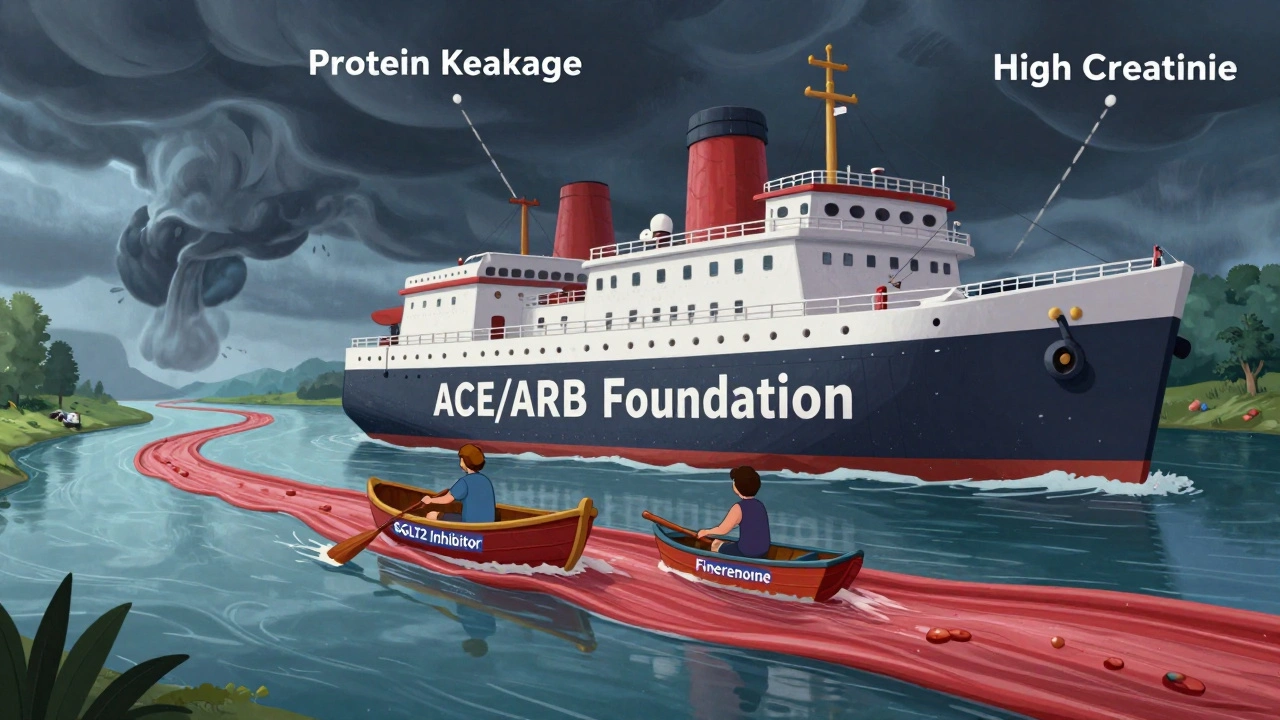
But here’s something new: SGLT2 inhibitors like empagliflozin and dapagliflozin are now being used alongside ACE inhibitors and ARBs. These drugs, originally for blood sugar, have shown powerful kidney protection on their own. But here’s the key: all major trials proving their benefit were done in patients already taking maximum-dose ACE inhibitors or ARBs. That means they’re add-ons, not replacements. The RAAS blockers still form the foundation.
Nonsteroidal mineralocorticoid receptor antagonists (MRAs) like finerenone are also showing promise, but again, they’re used on top of existing ACE inhibitor or ARB therapy. They’re not standalone treatments.
Biggest Mistakes Doctors and Patients Make
Despite decades of solid evidence, most patients still don’t get the right care. Studies show only 60 to 70% of people with diabetic kidney disease are even started on an ACE inhibitor or ARB after diagnosis. And of those who are, many are on doses too low to work.
Doctors often fear rising creatinine. Patients often stop the medicine because they feel fine. But feeling fine doesn’t mean your kidneys are safe. The real danger isn’t the small creatinine rise-it’s stopping the drug and letting protein leakage continue unchecked.
Another big mistake: combining these drugs with NSAIDs like ibuprofen or naproxen. These painkillers can cause sudden kidney injury, especially when used with diuretics like furosemide. If you need pain relief, talk to your doctor. Acetaminophen is usually safer.
What You Should Do Right Now
If you have diabetes and your urine test shows protein:
- Ask your doctor if you’re on an ACE inhibitor or ARB.
- If you are, ask what dose you’re on-and whether it’s the highest tolerated dose.
- If you’re not on one, ask why not.
- Don’t stop the medicine because your creatinine went up a little.
- Never take NSAIDs without checking with your doctor first.
- Get your urine protein checked every 3 to 6 months to track progress.
These drugs aren’t magic. They won’t fix everything. But if you’re on the right dose, they can delay kidney failure by years-or even prevent it. And that’s worth fighting for.
What’s Next in Treatment?
The future of diabetic nephropathy care isn’t about finding a new wonder drug. It’s about using what we already have correctly. The goal is to get everyone on a maximally tolerated ACE inhibitor or ARB-and keep them on it. Then, add SGLT2 inhibitors or MRAs if needed.
Research is also looking at how diet and lifestyle affect protein leakage. Lowering salt intake, controlling blood sugar tightly, and losing weight all help. But they don’t replace medication. They support it.
One thing is clear: we’ve had the tools for over 20 years. Now we just need to use them.
Can ACE inhibitors or ARBs reverse diabetic nephropathy?
They don’t reverse existing damage, but they can stop or dramatically slow further progression. Many patients see a significant drop in urine protein within weeks of starting the right dose. That’s the best sign the treatment is working.
Why is captopril the only ACE inhibitor FDA-approved for diabetic nephropathy?
Captopril was the first ACE inhibitor tested in large trials for diabetic kidney disease, so it got the official label. Other ACE inhibitors like ramipril and lisinopril have since been shown to be just as effective in multiple studies. The FDA approval doesn’t mean the others don’t work-it just means they weren’t submitted for that specific indication.
Is it safe to take an ACE inhibitor or ARB if I have stage 3 or 4 kidney disease?
Yes. In fact, guidelines now recommend them even when eGFR is below 30 mL/min/1.73 m². The benefits still outweigh the risks. The key is to monitor potassium and creatinine closely and adjust the dose if needed. Stopping them at this stage increases the risk of heart attack and faster kidney decline.
How long does it take to see results from ACE inhibitors or ARBs?
You might see a drop in urine protein within 2 to 4 weeks. Blood pressure usually drops faster. But kidney protection is a long-term game. The real benefit-slowing progression to dialysis-shows up over years, not months. Stay consistent.
Can I stop taking these drugs if my blood sugar improves?
No. Even if your A1C is perfect, the kidney damage from past high blood sugar doesn’t disappear. ACE inhibitors and ARBs protect your kidneys regardless of current blood sugar levels. Stopping them puts you back at risk. This isn’t a temporary fix-it’s lifelong protection.

So let me get this right… Big Pharma paid off the FDA to approve captopril ONLY so they could sell the rest at 10x the price?? And now they’re telling us to take MAXIMUM doses?? Who’s getting rich here? I’ve seen the ads-every single one says "protect your kidneys" but never mentions the $400/month copay… I’m not taking it until I see the receipts.
There’s a fundamental flaw in this narrative: the clinical trials were funded by pharmaceutical companies with vested interests. The RENAAL and IDNT studies? They excluded patients with comorbidities that might skew results. And the "30% reduction in kidney failure"-that’s relative risk, not absolute. For most patients, the actual benefit is closer to 2-3%. You’re being sold a placebo wrapped in jargon.
USA made these drugs, so of course they’re "the gold standard". In India, they use cheaper stuff and live longer. Also, why does every medical article now sound like a corporate press release? "Lifelong protection"? Sounds like a subscription service. I’ve got a cousin on dialysis-he never took these drugs. He eats curry, walks 5 miles a day, and still outlives his doctor.
What if the real problem isn’t the kidneys… but the idea that we need to "fix" them at all? We’ve turned a natural process into a disease to be conquered. Maybe protein in urine isn’t a sign of failure-it’s just your body saying, "I’m tired of this sugar tsunami." Maybe the answer isn’t more pills… but less denial. We’re treating symptoms like they’re enemies. But what if they’re messengers?
My uncle took losartan for 7 years. His creatinine went up 35%. Doctor told him to stop. He died 11 months later. Now I know: if your doctor tells you to stop because of creatinine… they don’t know what they’re doing. I’m on 100mg losartan. My protein is down. I don’t care if my kidneys "adjust"-I care that I’m still alive.
lol at people thinking ACE inhibitors are some miracle drug. My bro took ramipril for 2 years, got hyperkalemia, had to go to ER. Now he’s on amlodipine and feels better. Also, why do you think the FDA only approved captopril? Because it’s old and cheap. New drugs? They’re just rebranded crap. And don’t get me started on SGLT2 inhibitors-those are just diabetes drugs that got lucky in trials. Stop drinking the kool-aid.
Stop taking NSAIDs. Acetaminophen is fine. Check urine every 3 months. Take the dose. Don’t stop because creatinine rose. That’s it. No drama. No conspiracy. Just science. Do it.
Let me tell you something, folks-this isn’t medicine, it’s a WAR. Big Pharma is waging chemical warfare on our kidneys with their patented snake oil! They don’t care if you live or die-they care if you refill your prescription every 30 days! I’ve seen the documents! The FDA is a puppet! Captopril was approved because the CEO of Bristol-Myers Squibb had a golf game with the commissioner! And now they’re pushing SGLT2 inhibitors like they’re magic beans? HA! I’d rather drink bleach than take another one of these pills!
While I appreciate the clinical rigor of the referenced trials, I must express profound concern regarding the implicit moral imperative embedded in this article. The directive tone-"You must take this dose," "Never stop," "Always check"-imposes a coercive medical orthodoxy that undermines patient autonomy. One is left with the unsettling impression that adherence, not understanding, is the sole virtue. This is not healing; it is compliance engineering.
My doctor told me to take 100mg losartan… I cried. I was so scared. 😭 I thought I was going to die. But now? I feel like a warrior. My protein is down, my BP is perfect, and I’m not on dialysis. 💪 Thank you, science. 🙏 I’m not giving up. Ever. 💖