Gout Explained: How Purine Metabolism Causes High Uric Acid and What Medications Actually Work
Why Your Body Makes Too Much Uric Acid
When you eat meat, seafood, or drink beer, your body breaks down the purines in those foods. That’s normal. But in people with gout, something goes wrong in the process. Instead of clearing out the waste, your body lets uric acid build up-until it turns into sharp crystals in your joints. That’s what causes the sudden, burning pain in your big toe, ankle, or knee.
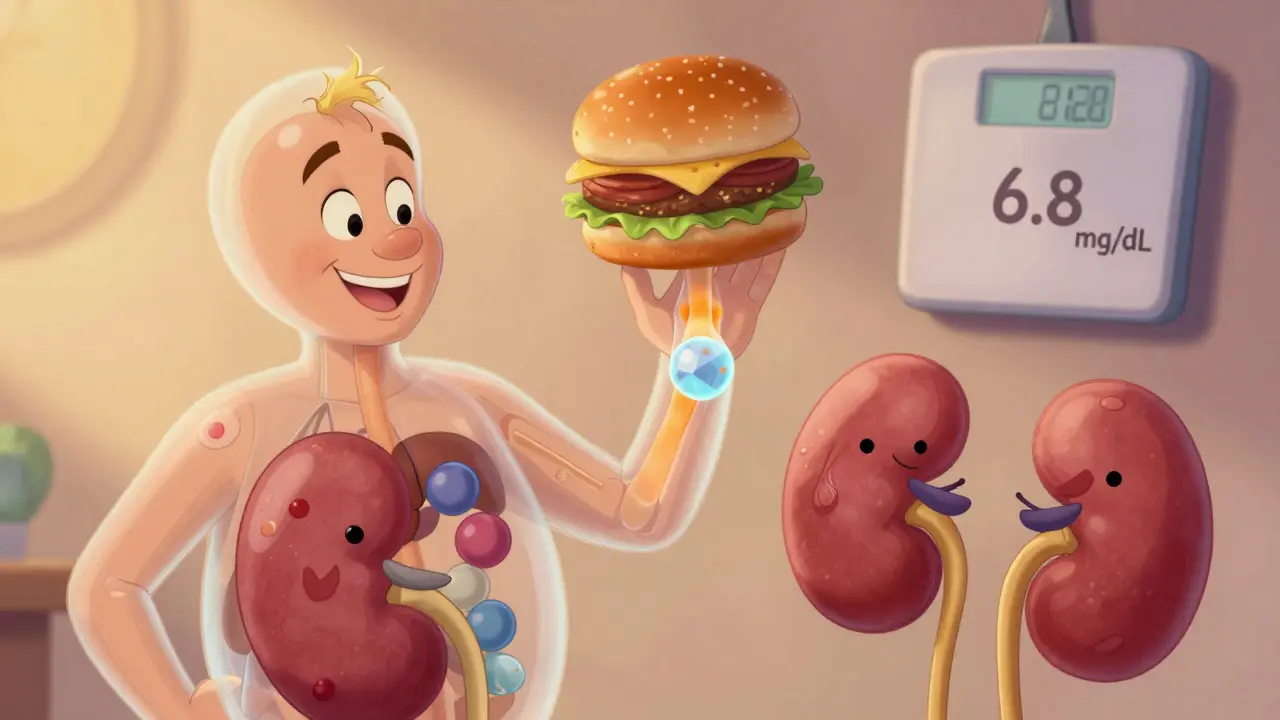
This isn’t just about diet. Gout is a metabolic disorder. Your body naturally produces uric acid as the final product of purine breakdown. Humans lost the enzyme uricase millions of years ago, so we can’t break it down further like other animals. That means all uric acid has to be cleared by your kidneys and gut. But if your kidneys aren’t excreting enough-or if your body is making too much-levels climb past 6.8 mg/dL. That’s the tipping point. Above that, crystals form. And once they do, your immune system attacks them, triggering inflammation, swelling, and pain.
How Purine Metabolism Actually Works
Here’s the simple version: purines from food or your own cells turn into uric acid in a three-step process. First, enzymes break down nucleotides into nucleosides. Then, those become hypoxanthine and guanine. Finally, xanthine oxidase turns them into uric acid. That last step is the key target for most gout medications.
But here’s the catch: about 65% of uric acid comes from your body’s own cells breaking down DNA and RNA-not from what you eat. That’s why cutting out steak won’t fix gout for most people. Even if you go vegan, your body still makes uric acid. The real problem is how much your body makes and how well your kidneys get rid of it.
Most of the uric acid your kidneys filter gets reabsorbed. Two transporters-URAT1 and GLUT9-pull it back into your blood. That’s why some drugs block these transporters. They don’t stop production. They help your kidneys flush it out.
The Three Types of Urate-Lowering Medications
There are three main classes of drugs used to lower uric acid long-term. Each works differently. And each has trade-offs.
Xanthine Oxidase Inhibitors (XOIs): Stop Production at the Source
These are the first-line treatment for 85% of patients. They block xanthine oxidase, the enzyme that turns xanthine into uric acid.
- Allopurinol: The oldest and cheapest. Generic versions cost about $4.27 a month. It’s effective, but most people don’t take enough. Doctors often start at 100 mg/day, but studies show you need to go up to 300 mg or higher to reach target levels. The 2020 ACR guidelines say titrating up is the #1 underused trick in gout care.
- Febuxostat: Stronger than allopurinol. At 80 mg/day, it gets 67% of patients to target uric acid levels. But it carries a black box warning from the FDA. The CARES trial found a higher risk of heart-related death compared to allopurinol. It’s not for people with heart disease unless there’s no other option.
Uricosurics: Help Your Kidneys Flush It Out
These drugs block URAT1, the transporter that pulls uric acid back into your blood. More gets peed out.
- Probenecid: Works well if your kidneys are healthy (eGFR above 50). But it’s useless if you have kidney disease. Also, it doesn’t work if your body is already making too much uric acid-only if your kidneys aren’t excreting enough.
- Lesinurad: Was approved in 2015 but pulled from the market in 2019. It boosted uric acid reduction when paired with allopurinol, but caused serious kidney damage in some patients.
Uricase Agents: Turn Uric Acid Into Something Harmless
Pegloticase is the only one in this class. It’s not a pill. It’s an IV infusion given every two weeks. It converts uric acid into allantoin, which your body easily flushes out.
- It works fast. In 6 months, 42% of patients hit target levels. For people with tophi (those visible lumps under the skin), it can dissolve them.
- But it costs over $16,000 a month. Insurance fights it. Many patients need 15+ appeals just to get it covered.
- It also triggers severe allergic reactions in 26% of users. You need to be pre-treated with steroids and antihistamines.
What Works Best? The Real-World Picture
Allopurinol is still the go-to. It’s cheap, proven, and safe for most people-if taken at the right dose. But here’s the problem: 92% of patients who take it at low doses never reach their target. That’s not the drug’s fault. It’s the dosing.
Febuxostat works better for people who can’t tolerate allopurinol or have severe kidney disease. But if you have heart disease, stick with allopurinol. The data is clear.
Pegloticase? It’s life-changing-for the small group with tophaceous gout who’ve tried everything else. But it’s not a first-line option. It’s a last resort.
On patient forums like MyGoutTeam and Reddit, the stories are mixed. One person says allopurinol gave them relief after years of pain. Another says they broke out in a rash and had to stop. Another says febuxostat raised their liver enzymes and they had to switch. No drug is perfect.

What You Can’t Ignore: Flares During Treatment
Here’s the big surprise: starting a urate-lowering drug can trigger gout flares. It sounds backwards, but it’s true. As crystals start to dissolve, your immune system gets confused. It sees the fragments and attacks.
The 2020 ACR guidelines say: Always start colchicine at the same time. Take 0.6 mg once or twice a day for at least six months, or until you’ve been flare-free for three months after reaching target uric acid. Many doctors skip this. Patients blame the medication. It’s not the drug. It’s the process.
Diet Matters-But Not Like You Think
Yes, organ meats, anchovies, and beer are high in purines. Liver has up to 400 mg per 100 grams. Anchovies: 500 mg. Beer: 10-20 grams per liter.
But here’s the truth: diet alone usually lowers uric acid by only 1-2 mg/dL. That’s not enough to get most people below 6.0 mg/dL. So don’t think cutting out shellfish will cure your gout. It helps. But it’s not the fix.
What matters more? Weight loss. Alcohol (especially beer and spirits). Sugary drinks. If you’re overweight and drink soda daily, fixing those two things will help more than going gluten-free.
Why Most People Stop Taking Their Meds
A 2022 survey found 61% of gout patients quit their urate-lowering meds within a year. Why?
- 33% said it didn’t seem to work.
- 29% had side effects-rash, nausea, liver issues.
- 18% said the dosing was too confusing.
That’s the real crisis. Not the drugs. The system. Most patients get a prescription and are told to take it daily. No follow-up. No blood tests. No dose adjustments. They don’t know their uric acid level. They don’t know what target they’re supposed to hit. So they stop.
Only 29% of primary care doctors check uric acid levels regularly after starting treatment. That’s not enough.
What’s Coming Next
The future of gout treatment is getting smarter.
- Verinurad: A new URAT1 blocker in Phase III trials. Early data shows it cuts uric acid even more when combined with febuxostat.
- Arhalofenate: A dual-action drug that lowers uric acid and reduces inflammation. Early results show fewer flares.
- Personalized medicine: Researchers are looking at genetic markers like SLC2A9 variants to predict who responds best to which drug.
- Longer-acting uricase: One shot a month instead of two weeks? That’s the goal.
What You Should Do Right Now
If you have gout:
- Ask your doctor for your last serum uric acid level. If you don’t know it, get it tested.
- If you’re on allopurinol, ask: "Is my dose high enough?" Most people need 300 mg or more.
- Ask if you should be taking colchicine daily to prevent flares.
- Get your kidney function checked (eGFR).
- If you have heart disease, avoid febuxostat unless your doctor says it’s your only option.
- Track your triggers: alcohol, red meat, sugary drinks, stress.
Gout isn’t just about pain. It’s a warning sign. High uric acid is linked to kidney disease, heart disease, and diabetes. Treating it isn’t optional. It’s essential.
How Often Should You Get Tested?
When you start a new medication, check your uric acid every 2-5 weeks until you hit target (<6.0 mg/dL). Once you’re stable, check every 6 months. That’s the standard. If your doctor isn’t doing this, ask why.
What If I Can’t Afford My Meds?
Allopurinol is $4 a month. That’s affordable. Febuxostat is $60. That’s harder. Pegloticase? Over $16,000. If you need it, work with your rheumatologist and pharmacy. Many drug companies have patient assistance programs. Insurers often require prior authorization-but persistence pays off. One patient on Reddit got approved after 17 appeals. It took a year. But his tophi disappeared.
Final Thought
Gout used to be called the "disease of kings." Now it’s the disease of modern diets, obesity, and neglected care. But it’s one of the most treatable forms of arthritis-if you treat it right. It’s not about avoiding shrimp. It’s about taking the right dose of the right drug, monitoring your levels, and staying on it. That’s the only way to stop the pain, dissolve the crystals, and protect your kidneys and heart.

Wow, so you're telling me I've been blaming my beer for 10 years but it's actually my kidneys being lazy? I mean, I get it, but come on. I didn't sign up for a lifetime of pills just because my body refuses to cooperate. I'm not even overweight. This feels like a scam. I'm done listening to doctors who think I'm just a walking uric acid factory.
Thanks for laying this out so clearly. I've been on allopurinol for 3 years and never knew I needed to bump up the dose. My doc just gave me 100mg and said 'take it daily.' No follow-up, no labs. I thought the drug wasn't working. Turns out I was just underdosed. I'm going to ask for a titration next week. Also, colchicine for flares? I had no idea that was standard. This post saved me from quitting meds again.
Let me guess-Big Pharma wrote this. Xanthine oxidase inhibitors? Sure. But why no mention of glyphosate? The weedkiller in your food and water? It shuts down your kidneys’ ability to excrete uric acid. That’s the real culprit. Allopurinol? Just a Band-Aid. They don’t want you to know that your gout is caused by Roundup in your corn syrup and processed meats. The FDA’s black box warning on febuxostat? That’s because they’re covering for the real villain. Google ‘uric acid glyphosate study’ and you’ll see. They buried it.
Bro. I was in so much pain I couldn’t walk. Tried the diet thing-no beer, no shrimp, vegan for 3 months. Still flaring. Then my rheumy upped my allopurinol to 300mg and put me on daily colchicine. Two weeks later? Zero flares. For the first time in 7 years. Don’t listen to the internet gurus. If you’re on less than 300mg and still flaring, you’re doing it wrong. Also, stop drinking soda. Seriously. Even diet. It’s worse than beer.
Man… this hits different. I used to think gout was just ‘old man pain’ until I got it at 34. I thought it was punishment for eating too much pizza 🍕. But reading this… it’s not about guilt. It’s biology. We lost uricase. Our bodies are stuck with this ancient, inefficient system. And now we’re expected to fix it with pills and willpower? No wonder people quit. We need better systems-not just better drugs. Maybe one day we’ll have a pill that fixes the transporter problem without killing your kidneys. Until then… I’m taking my colchicine. And yes, I’m drinking water like it’s my job 💧
Everyone’s talking about allopurinol like it’s magic. But what about the people who get Stevens-Johnson? The rashes? The hospitalizations? You think it’s just ‘dosing’? No. It’s genetic. Some of us are just built to break down. You’re not helping by pushing meds like they’re candy. I lost my cousin to a reaction. You don’t get to tell people to ‘just take more’ when their body says NO.
Correction: The 2020 ACR guidelines recommend titrating allopurinol to achieve a serum uric acid level below 6.0 mg/dL, not merely ‘300 mg or higher.’ The dose is patient-specific and depends on renal function, weight, and baseline uric acid. Stating ‘most people need 300 mg or more’ is misleading. Additionally, the CARES trial’s increased cardiovascular mortality risk was only observed in patients with preexisting cardiovascular disease-this nuance is critical and omitted here. Precision matters.
Pegloticase is the only uricase agent available and it converts uric acid to allantoin via recombinant porcine enzyme which is immunogenic hence the high rate of infusion reactions and need for premedication with steroids and antihistamines also the cost is prohibitive and insurance denials are common due to lack of step therapy compliance and insufficient documentation of treatment failure with XOIs and uricosurics