How Generic Combinations Save Money: Comparing Individual Generics vs. Combination Drugs

When you pick up a prescription, you might assume all generics are created equal. But that’s not true. Some generic drugs cost 15 times more than other generics that do the exact same thing. And when you compare single-drug generics to combination products, the savings can be even bigger-sometimes over 90%.
Why Some Generics Are Way More Expensive Than Others
Not all generics are cheap. A 2022 study of 1,000 top-selling generics in Colorado found 45 of them were shockingly expensive-far pricier than other drugs that work just as well. One example: a generic version of a common blood pressure pill was priced at $7.50 per dose, while another generic with the same active ingredient cost just $0.40. That’s a 95% difference for the same effect. The reason? It’s not about quality. It’s about competition. When only one company makes a generic, they can keep prices high. But when five or six companies start making the same drug, prices crash. The FDA found that with three or more generic makers, prices drop by about 20% in three years. With ten competitors? You’re looking at 80% off the original brand price. Take Crestor. When the brand-name version lost patent protection in 2015, the price per pill dropped from $5.78 to just $0.08. That’s a 99% drop. Prilosec followed the same path: from $3.31 to $0.05. These aren’t rare cases. They’re the rule when enough manufacturers enter the market.Combination Drugs: One Pill, Big Savings
Combination drugs-medications that pack two or more active ingredients into one pill-are often cheaper than buying each drug separately. This isn’t just convenient. It’s financially smarter. Take asthma inhalers. Before generic versions of Advair Diskus hit the market, patients paid around $334 per inhaler. Then Wixela Inhub, a generic combination of the same two drugs (fluticasone and salmeterol), arrived. The price dropped to $115. That’s a 66% cut in cost per prescription. Across the U.S., monthly spending on Advair and its generics fell from $337 million to $233 million in just one year. That’s over $1 billion saved annually. The same pattern shows up in diabetes, high blood pressure, and arthritis. A single pill with metformin and sitagliptin costs less than buying metformin and sitagliptin separately. Same with lisinopril and hydrochlorothiazide for blood pressure. Why? Manufacturing, packaging, and distribution costs are shared. Pharmacies and insurers prefer them because they’re easier to manage-and cheaper.Therapeutic Substitution: Swap the Drug, Not the Result
You don’t always need to stick to the exact generic your doctor prescribed. Sometimes, switching to a different generic-same active ingredient, different strength or form-can slash your bill. The Colorado study found that 62% of high-cost generics could be replaced with a lower-cost version of the same drug, just in a different dosage. For example, switching from a 10mg tablet to a 5mg tablet (and taking two) saved 95% on average. Or switching from a capsule to a tablet. These aren’t experimental swaps. They’re FDA-approved and clinically identical. Your pharmacist can help. The FDA’s Orange Book lists which generics are rated as therapeutically equivalent (marked with an “A”). If your prescription says “A,” you can safely swap it for another “A” rated version-even if it’s made by a different company. Ask your pharmacist: “Is there a cheaper generic that works the same?”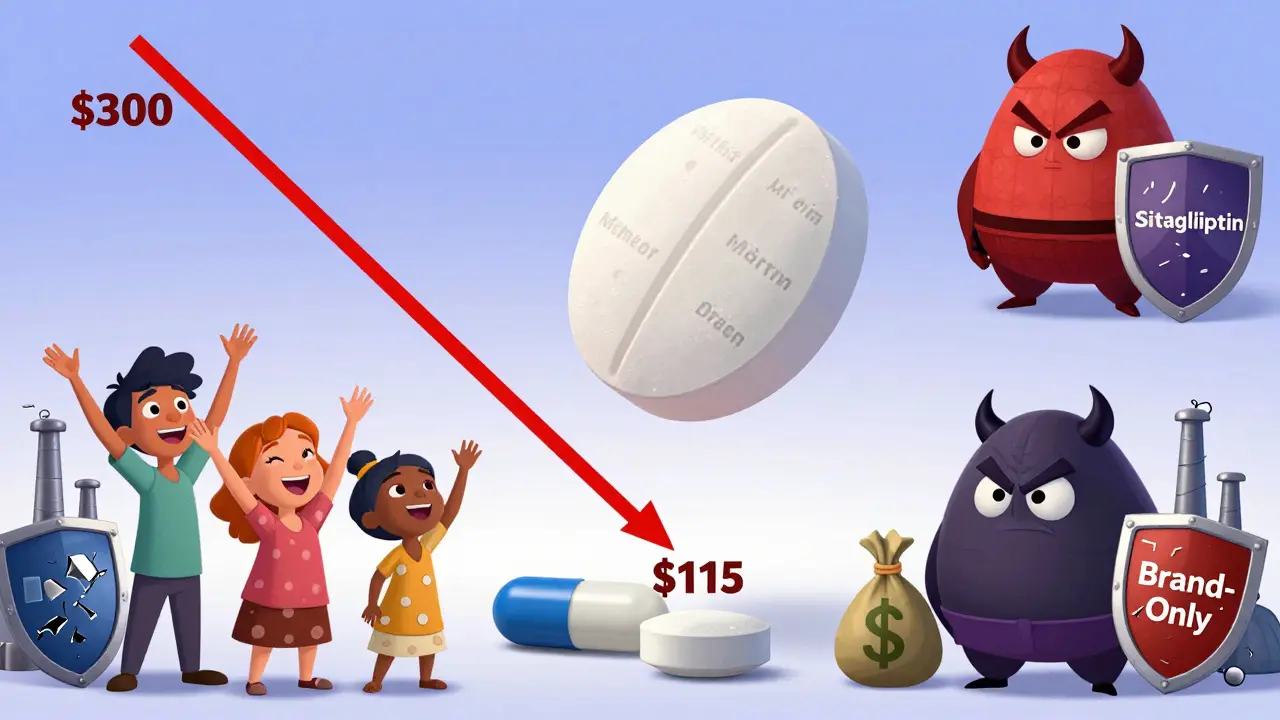
Who Saves the Most? Uninsured Patients See the Biggest Gains
Savings aren’t spread evenly. A 2023 study of nearly 844 million prescriptions found that uninsured patients saved the most. On average, they paid $6.08 less per prescription when switching to a lower-cost generic. That’s because they’re paying full price-no insurance cushion. For them, a $10 saving isn’t just a number. It’s a meal, a bus ticket, or a skipped co-pay. Medicare patients saved $4.64 per script. Private insurance saved $3.69. Medicaid patients? Almost no savings were found. Why? Because Medicaid already negotiates deep discounts upfront. There’s not much room to go lower. The bottom line: if you’re paying out-of-pocket, your savings potential is huge. If you’re on Medicare or private insurance, you’re still saving-just less dramatically. Either way, asking “Is there a cheaper option?” is always worth it.Why Aren’t More People Doing This?
You’d think everyone would switch to the cheapest generic. But barriers exist. Some doctors don’t know about the price differences. Others are used to prescribing one brand of generic and don’t think to change. Pharmacies sometimes stock only the most expensive version because their supplier pushed it. And sometimes, insurance plans don’t update their formularies fast enough. Also, some companies use tricks to keep prices high. They tweak the pill shape, change the inactive ingredients, or file small patents to delay competition. These aren’t new drugs-they’re just slight changes to keep the cash flowing. The fix? Plan sponsors (like employers or insurers) should review their top 20 most expensive generics every quarter. Look for drugs where a cheaper alternative exists. Push for formulary changes. Educate prescribers. And empower pharmacists to suggest swaps.
What You Can Do Right Now
You don’t need a degree in pharmacology to save money on generics. Here’s what works:- Ask your pharmacist: “Is there a lower-cost generic version of this drug?”
- Check if your drug is a combination product. If you’re taking two pills, ask if one combination pill exists.
- Don’t assume your current generic is the cheapest. Compare prices at different pharmacies-even Walmart and Costco often beat specialty pharmacies.
- If you’re uninsured or on Medicare, use services like Mark Cuban Cost Plus Drug Company or GoodRx. They show real-time cash prices.
- Request the FDA’s Orange Book ratings if you’re unsure if two generics are interchangeable.

I used to pay $80 for my blood pressure med until I switched to the $0.50 generic. My pharmacist showed me the Orange Book rating and I was shocked. Same active ingredient, same results. I wish more people knew this stuff.
It’s not magic, it’s just basic math. Why pay 15x more for the same pill?
AMERICA IS GETTING ROBBED. These big pharma companies are laughing all the way to the bank while normal people struggle to afford insulin. Why is the FDA letting this happen? This is why we need to break up the drug monopolies and bring manufacturing back to the U.S. 💪🇺🇸
And stop buying foreign generics! I don’t care if they’re ‘FDA approved’-I want American-made pills!
It is an incontrovertible fact that the commodification of pharmaceuticals has led to a profound disjunction between therapeutic efficacy and economic accessibility. The market mechanism, when unregulated by ethical imperatives, inevitably privileges profit over public health.
One might posit that the disparity in pricing among therapeutically equivalent generics constitutes a form of structural injustice, wherein the most vulnerable populations bear the greatest burden of systemic inefficiency.
Wait… so you’re telling me the government knows about this but lets it happen? 😏
Big Pharma owns the FDA, the doctors, the pharmacies, and even the Orange Book. They’re making us take the same pill in a different color so they can charge more. And they call it ‘new formulation.’
Remember when they said 5G caused COVID? Same playbook. They’re not trying to heal you. They’re trying to keep you hooked. 💊👁️
Also, I heard the moon landing was fake. Coincidence? I think not.
This is such a game-changer! I feel so empowered just reading this.
My mom used to pay $120 for her diabetes meds until she switched to the combo pill-now it’s $18. She cried happy tears. You don’t need to be a genius to save money-you just need to ask the right questions.
Pharmacists are heroes. Talk to them. Don’t be shy. You’re not bothering them. You’re helping them help you.
And if you’re struggling? There are programs. There are discounts. There are people who want you to be okay. You’re not alone. 💛
Just a quick note: if you’re on Medicare Part D, check your plan’s formulary every year during open enrollment. The cheapest generic one year might not be covered the next.
Also, GoodRx coupons often work even if you have insurance-sometimes better. I’ve saved $40 on a single script by using it. No tricks, just facts.
And yes, splitting pills (with your doctor’s approval) is totally safe for many meds. I did it with my antidepressant and saved $60/month. Small changes add up.
I used to work in a pharmacy and let me tell you-the real story isn’t even in the data. It’s in the quiet moments.
Like the elderly woman who came in crying because she was skipping doses to make her $80 pill last longer. Or the guy who told me he was choosing between his meds and his kid’s school supplies.
We had shelves full of identical pills-same chemical, same effect, different price tags. And we were told to push the expensive ones because the distributor gave us better margins.
It broke my heart. I started keeping a little list of cheaper alternatives. I’d slip it into the bag. No fanfare. Just… here, this one’s $2. You’ll be fine.
People don’t know. They think the price means something. It doesn’t. It just means someone else is making money off their fear.
Competition drives price down. That’s economics 101. But when you have monopolistic control over a life-sustaining commodity, the market fails.
Generics aren’t the problem. The system is.
Why do we allow patent evergreening? Why do we let one company control the supply chain for a drug with 10+ manufacturers capable of producing it?
The answer isn’t individual action. It’s structural reform. But since that’s unlikely, we do what we can. Ask. Compare. Swap. Persist.
Let’s be clear: the entire generic drug paradigm is a neoliberal farce engineered to create the illusion of affordability while consolidating oligopolistic control.
The FDA’s Orange Book is a performative artifact-its ‘A’ ratings are statistically meaningless when supply chains are vertically integrated under three multinational conglomerates.
Moreover, the notion that ‘switching’ to a 5mg tablet constitutes ‘savings’ is a gross misrepresentation of pharmacoeconomic agency. It shifts responsibility from systemic failure to patient labor.
And don’t get me started on GoodRx. It’s a data-mining Trojan horse disguised as a discount platform. Your prescription history is being sold to insurers who then adjust your premiums accordingly.
True savings? Nationalize pharmaceutical production. End patent monopolies. Period.
As a Black man who’s seen family members skip meds because they cost more than groceries-I’m so glad this got posted.
But here’s the truth: this isn’t just about pills. It’s about dignity.
When you’re poor, every dollar is a decision. When you’re Black or Brown or immigrant, you’re often treated like you don’t deserve to be healthy.
So yes-ask your pharmacist. Use GoodRx. Split pills if safe. But also-demand better. Talk to your reps. Support policies that force transparency.
We don’t need to be heroes. We just need to stop being silent.
Therapeutic equivalence, as defined by the FDA’s Orange Book, is codified under the AB rating system. An ‘A’ rating indicates bioequivalence, meaning the drug has the same active ingredient, strength, dosage form, and route of administration, and demonstrates comparable bioavailability within statistically acceptable limits.
However, excipient variation may affect patient tolerance, particularly in those with sensitivities to dyes, lactose, or gluten. While pharmacokinetic equivalence is established, pharmacodynamic equivalence is not always assessed in post-market surveillance.
Therefore, while cost-savings are substantial, clinicians should remain cognizant of individual patient-specific factors when recommending substitutions.