Latanoprost for Pediatric Glaucoma: A Comprehensive Guide
Understanding Pediatric Glaucoma
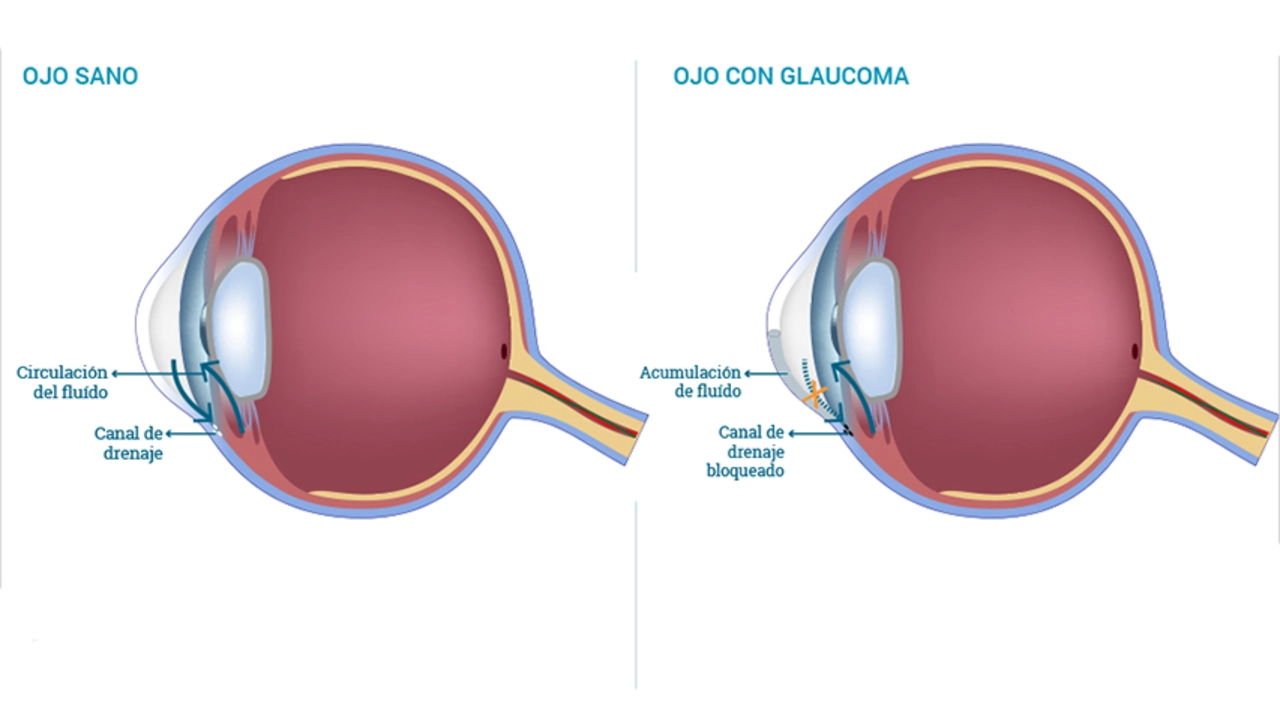
Before diving deep into the topic of Latanoprost for pediatric glaucoma, let's first understand what pediatric glaucoma is. Pediatric glaucoma, also known as childhood glaucoma, is a rare and severe condition that affects children. It can cause permanent vision loss if not treated promptly. Unlike adult glaucoma, which usually develops slowly over time, pediatric glaucoma often appears shortly after birth or in the first few years of life. The symptoms can include excessive tearing, light sensitivity, and a cloudy appearance of the eye.
What is Latanoprost?
Latanoprost is a medication that falls in the class of drugs known as prostaglandin analogs. It is mainly used to treat certain types of glaucoma and other causes of high pressure inside the eyes. It works by increasing the outflow of natural eye fluids, thereby reducing the pressure within the eye. It is typically administered in the form of eye drops and can be used in both adults and children.
Benefits of Latanoprost for Pediatric Glaucoma
Latanoprost has several benefits when used in the treatment of pediatric glaucoma. Firstly, it is a once-daily medication, which can make it easier for parents to administer. Secondly, compared to other glaucoma medications, it has fewer systemic side effects, which can be particularly important in children. It also has been shown to be effective in reducing intraocular pressure in children, which is crucial in preventing vision loss from glaucoma.
How to Administer Latanoprost
The administration of latanoprost can be a bit tricky, especially for young children, but with a little practice, parents can quickly get the hang of it. The medication usually comes in the form of eye drops, and it should be applied to the affected eye(s) once a day, in the evening. Care should be taken to avoid touching the dropper tip to any surface, to prevent contamination. After the drops have been applied, the child should close their eyes for a minute or two to let the drops absorb.
Side Effects of Latanoprost
Like any medication, latanoprost can have side effects. The most common side effects include redness or discomfort of the eyes, blurred vision, and changes in eyelash length or color. In some cases, it can also cause a gradual change in the color of the eyes. While these side effects can be concerning, they are usually mild and go away on their own. However, if they persist or worsen, it's important to contact your healthcare provider.
Precautions when Using Latanoprost
Before using latanoprost, it's important to discuss any allergies your child may have with your healthcare provider, as latanoprost can cause allergic reactions in some individuals. Also, certain medical conditions, such as a history of eye inflammation or macular edema, can make the use of latanoprost riskier. If your child wears contact lenses, they should be removed before applying the drops, as latanoprost can be absorbed by the lenses.
Alternatives to Latanoprost
In cases where latanoprost is not effective or well-tolerated, there are other treatment options available for pediatric glaucoma. Other classes of eye drops such as beta-blockers, carbonic anhydrase inhibitors, or alpha agonists can also be considered. In some cases, surgical procedures may be recommended. The best treatment for each child will depend on their individual condition and response to medication, and should be discussed thoroughly with their healthcare provider.

The article correctly outlines the mechanism of Latanoprost and its dosing schedule. It is important to emphasize that parental compliance is essential for therapeutic success. Monitoring intraocular pressure regularly remains a key practice.
Wow this drug sounds like a miracle for kids!
While the piece is thorough, it glosses over the potential for prostaglandin‑induced iris pigmentation changes. Those side effects deserve a more critical discussion.
Great summary! I especially appreciate the tip about letting the child keep the eyes closed briefly after instillation. This simple step can improve drug absorption. Keep sharing such practical guidance.
Looks like another pharma push, but hey if it works, why complain.
In many South Asian families, eye‑drop routines are integrated with bedtime prayers, which helps children remember the schedule. It also offers an opportunity to involve grandparents in care. Such cultural practices can boost adherence.
The composition of this guide, while ostensibly comprehensive, lacks the peppered nuance expected of a truly scholarly discourse. One pines for a deeper exploration of comparative pharmacodynamics. Moreover, the omission of cost‑effectiveness analyses is a glaring oversight. The reader is left navigating a shallow pond when a deeper ocean beckons. Perhaps future revisions will amend these lacunae.
From a clinical workflow perspective, incorporating Latanoprost into the pediatric regimen simplifies the therapeutic algorithm. The once‑daily dosing reduces the burden on nursing staff and allows for streamlined documentation. This aligns with best‑practice protocols for chronic ophthalmic management.
I have to say that after reading this, I am left with a mixed feeling. On the one hand the guide does a decent job of covering the basics of pediatric glaucoma and the role of prostaglandin analogs. On the other hand, the narrative drifts into repetitive territory, especially when describing the administration technique. It would have benefitted from a concise bullet list rather than verbose paragraphs. The side‑effect profile was mentioned, yet the clinical significance of each was barely touched upon. Parents may find themselves searching elsewhere for deeper insight. Still, the inclusion of precautionary advice is commendable. Overall, it feels like a well‑intentioned but somewhat pedestrian effort.
Everything about eye drops is a government experiment.
This is fluff, stop.
Thanks for the clear steps. They’ll make it easier for families. Keep up the good work.
Honestly, the so‑called 'clinical workflow' nonsense is just lazy British jargon!!! 👎🇺🇸
Your disdain betrays a narrow worldview; a truly erudite discourse would rise above such petty bravado.
It is with a profound sense of gravitas that I approach the subject of Latanoprost administration in the delicate cohort of pediatric patients. The author, in their earnest endeavor, has assembled a compendium of salient points that merit both commendation and measured critique. Firstly, the exposition concerning the pharmacodynamic pathway of prostaglandin analogs is articulated with commendable clarity, thereby furnishing the reader with a foundational understanding. Nonetheless, the treatise omits a thorough deliberation on the pharmacokinetic variability observed across differing ages and ocular physiologies, a lacuna that warrants immediate redress. Moreover, the counsel to eschew contact lens wear during instillation, while prudent, is presented without an accompanying discussion of the temporal parameters for lens reinsertion, leaving practitioners to infer a protocol. The segment addressing adverse ocular pigmentation, albeit concise, fails to contextualize the prevalence statistics against a backdrop of long‑term aesthetic considerations for the child. In a similar vein, the narrative’s cursory reference to potential macular edema is insufficient, as the condition, albeit rare, carries significant visual implications. The recommendation of a solitary evening dose aligns with circadian rhythms of aqueous humor production, yet the article neglects to mention the impact of bedtime variances on therapeutic efficacy. From a pedagogical perspective, the inclusion of a mnemonic device or visual aid could have augmented retention for caregivers, an aspect conspicuously absent. The discourse, while generally methodical, occasionally succumbs to redundant phrasing, particularly within the procedural instructions. A more streamlined, bullet‑point format would enhance readability for the lay audience. Lastly, the omission of cost‑effectiveness analysis, especially pertinent in resource‑limited settings, represents a missed opportunity to broaden the guide’s applicability. In summation, while the guide constitutes a valuable primer, these identified deficiencies suggest avenues for refinement, thereby elevating its utility for both clinicians and families alike.
I wonder how the long‑term ocular surface health is affected by nightly instillation. Could there be cumulative effects on the corneal epithelium? It would be valuable to see longitudinal studies addressing this. Also, the role of genetic predisposition in response variability intrigues me. Perhaps future research will shed light on these aspects.
Guys, remember that consistency beats perfection. Even if a drop misses the eye once, just keep going. Encourage the kids with small rewards and make it a game. That attitude can really improve outcomes.
The article seems to ignore the cost barrier for many families, which is a significant oversight.
Maybe we could add a quick checklist for parents at the end of the guide? Something like: drop, close eyes, wait two minutes, log the time. That would make it more actionable.
Nice overview, thanks.