PCI vs. CABG: Which Coronary Revascularization Option Is Right for You?
When your heart arteries are clogged, two main options exist: PCI and CABG. Neither is "better" across the board. The right choice depends on your specific heart anatomy, health conditions, and what matters most to you - quick recovery or long-term peace of mind.
Let’s cut through the noise. You’re not just choosing between a stent and a bypass. You’re deciding how you want to live for the next 10, 15, even 20 years. One path gets you back to work in days. The other might mean months of healing, but it could keep you pain-free for life. This isn’t theoretical. Real people face this every day. And the data doesn’t lie.
Percutaneous Coronary Intervention (PCI), commonly called angioplasty with stent, is a minimally invasive procedure. A thin tube is threaded through an artery in your wrist or groin, up to your heart. A tiny balloon opens the blockage, and a metal mesh stent - usually coated with medicine - holds it open. It’s done under local anesthesia. Most people go home the next day. In 2023, over 600,000 PCIs were done in the U.S. alone. It’s fast. It’s common. But it’s not always the longest-lasting fix.
Coronary Artery Bypass Grafting (CABG) is open-heart surgery. Surgeons take a healthy blood vessel - often from your chest, leg, or arm - and use it to create a detour around the blocked artery. The most effective graft is the left internal mammary artery (LIMA) connected to the left anterior descending (LAD) artery. This is the highway of the heart. When done right, LIMA grafts stay open 90% of the time after 10 years. CABG takes 3 to 6 hours. Recovery? At least a week in the hospital. Six to eight weeks before you feel normal again. But for many, it’s the only way to truly stop the disease in its tracks.
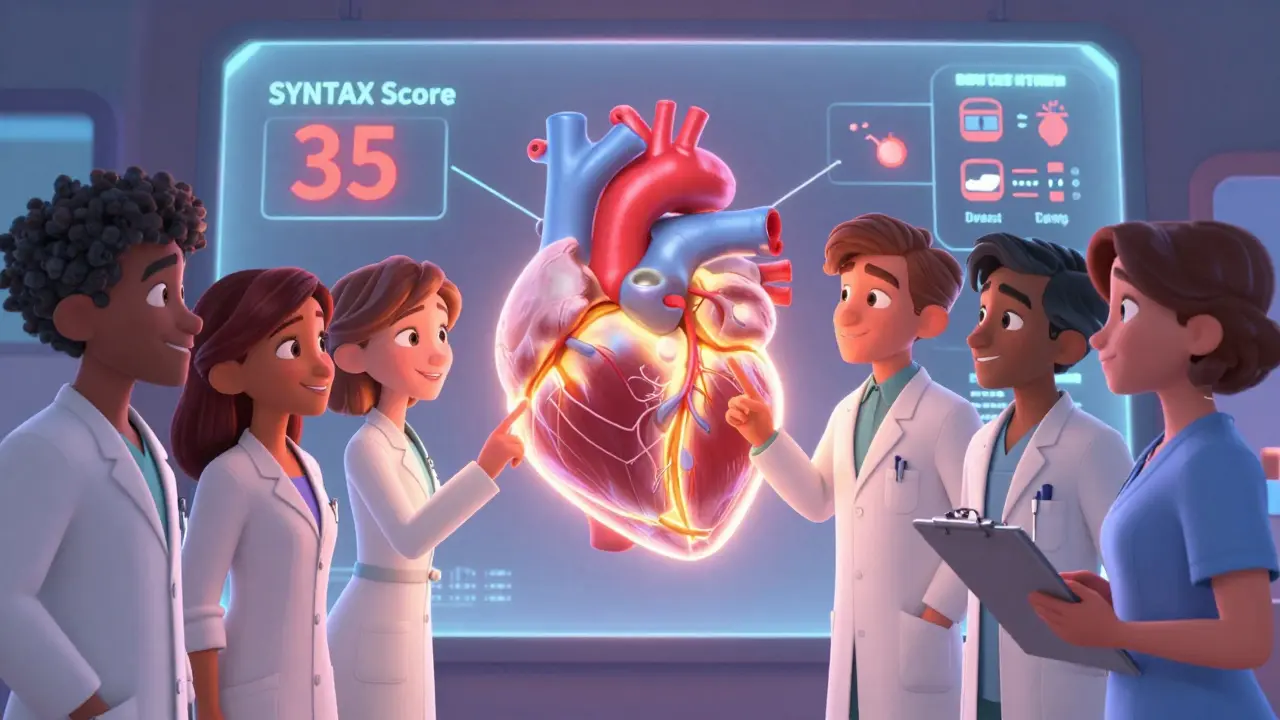
Why the SYNTAX Score Matters More Than You Think
Doctors don’t pick PCI or CABG based on gut feeling. They use a tool called the SYNTAX Score. It’s a detailed map of your coronary arteries, scored based on how many blockages you have, where they are, and how bad they are. Think of it like a road atlas for your heart.
- Score under 22: PCI is usually the go-to. Your blockages are simpler, more isolated. Stents work great here.
- Score between 22 and 32: This is the gray zone. Your heart team will dig deep into your age, diabetes status, kidney function, and even your job. No one-size-fits-all.
- Score over 32: CABG wins. Complex, multi-vessel disease with long, calcified blockages? Surgery gives you the best shot at survival and avoiding repeat procedures.
The SYNTAX trial in 2009 showed that for patients with scores above 32, CABG cut major heart events by nearly 35% compared to PCI over five years. And repeat procedures? Half as likely. That’s not a small edge. That’s life-changing.
Diabetes Changes Everything
If you have diabetes, the rules shift dramatically. The FREEDOM trial - one of the most important studies in modern cardiology - proved it. In diabetic patients with multi-vessel disease, those who got CABG had a 40% lower risk of dying over five years than those who got stents. The numbers? 10% died after CABG. 16.4% died after PCI. That’s not a margin. That’s a canyon.
Why? Diabetes damages blood vessels everywhere. Stents work in the short term, but they’re more likely to re-narrow in diabetic patients. CABG, especially with arterial grafts, creates a durable bypass that ignores the disease process. The American College of Cardiology now gives CABG a Class IA recommendation - the strongest possible - for diabetics with multi-vessel disease involving the LAD. If you’re diabetic and have more than one blocked artery, this isn’t a suggestion. It’s the standard of care.
Left Main Disease: The Tipping Point
The left main artery supplies most of the left side of your heart. Block it, and you’re one heartbeat away from a massive heart attack. Treating left main disease is high-stakes. For years, CABG was the only accepted option. Then came the EXCEL and NOBLE trials.
EXCEL showed that at three years, PCI and CABG were nearly equal in safety for left main disease. But here’s what they didn’t tell you at first: by year five, CABG pulled ahead. The risk of death, heart attack, or needing another procedure was 61% higher with PCI after the first 30 days. That’s not a glitch. That’s the long-term truth.
NOBLE found the same pattern: more repeat procedures with PCI, but no big difference in death rates. So what’s the takeaway? If you’re young, active, and want to avoid repeat surgeries, CABG is the safer long-term bet. If you’re older, frail, or can’t handle major surgery, PCI might be the only realistic option - even if it means you’ll likely need another procedure down the line.
Recovery: Fast vs. Lasting
Let’s talk about the real cost of each choice - your time.
After PCI, most people are back to light duties in 2 to 3 days. The VA CART registry found 87% of PCI patients returned to work within two weeks. No large incision. No sternal pain. You can drive, cook, walk the dog - soon.
But CABG? It’s a different story. You’ll be in the hospital for 5 to 7 days. Your sternum is cut open and wired back together. Pain is real. At three months, nearly half of CABG patients still feel chest discomfort. At six weeks, you’re still avoiding lifting anything heavier than a coffee mug.
Yet here’s the twist: by six months, 94% of both groups are back to work. And at one year, CABG patients report better quality of life. The ROSETTA trial found 92% of CABG patients had complete relief from chest pain. Only 85% of PCI patients did. Why? Because stents can fail. Grafts, especially arterial ones, don’t.
One patient on Reddit said: "Six weeks of recovery was tough, but two years later I’m hiking again with no chest pain." Another said: "Back to work in three days - but needed another stent after 18 months." Both are true. Both matter.
Stroke Risk: The Hidden Trade-Off
There’s a catch with CABG: stroke risk. During surgery, tiny clots or air bubbles can travel to the brain. The Palmerini meta-analysis found CABG had a 1.7% stroke rate at five years. PCI? Just 1%. That’s a 73% higher risk with surgery.
But here’s the context: most strokes after CABG happen in the first week. And they’re often mild. Most patients recover fully. Meanwhile, PCI’s lower stroke risk comes with a higher risk of heart attack later - especially if you’re diabetic or have complex disease.
So if you’re 75 with a history of mini-strokes? PCI might be safer. If you’re 60 with diabetes and three blocked arteries? The long-term heart protection from CABG outweighs the small stroke risk.

The Heart Team: Why You Need More Than One Doctor
Too many patients are handed a pamphlet and told to pick. That’s not enough. The 2021 ACC/AHA guidelines say revascularization decisions must be made by a heart team - a cardiologist who does stents, a surgeon who does bypasses, and often a nurse, anesthesiologist, or heart failure specialist.
Why? Because each specialist has a bias. The interventional cardiologist sees stents as the solution. The surgeon sees surgery as the gold standard. The heart team forces them to look at the whole picture: your age, your kidneys, your lungs, your ability to recover, your goals.
Only 42% of community hospitals have formal heart teams. If yours doesn’t, ask for a referral to a center that does. This isn’t bureaucracy. It’s survival.
What’s Next? The Future of Revascularization
Technology is changing fast. Bioresorbable stents - which dissolve after healing - are being redesigned. Robotic-assisted CABG is cutting recovery time. Hybrid procedures - combining a single bypass with a stent - are showing promise in early trials.
But the biggest shift isn’t tech. It’s mindset. We’re moving away from "one procedure fits all" to "what’s best for you, right now, and in 10 years?"
The American Heart Association predicts CABG volumes will stay steady at 280,000-300,000 a year through 2030. Not because it’s outdated - but because it’s still the best option for the most complex cases. PCI will grow, not because it’s better, but because more people live longer with heart disease, and they want a quick fix.
But quick fixes don’t always last. And when they fail, you’re back to square one - with more scar tissue, more risk, and fewer options.
What Should You Do?
If you’re facing this decision:
- Get your SYNTAX score. Don’t accept vague terms like "severe blockage." Ask for the number.
- If you have diabetes, push for CABG unless you’re too high-risk for surgery.
- If your blockages are simple (SYNTAX <22), PCI is fine - but know you might need another one.
- Insist on a heart team meeting. Don’t let them rush you.
- Ask: "If this were your parent, what would you recommend?"
There’s no perfect choice. But there is a right choice - for you. And it’s not about what’s trendy. It’s about what keeps your heart beating strong for decades to come.

I just got my SYNTAX score back-28. I’m diabetic. My cardiologist said "PCI is fine." But I read this and now I’m scared. I don’t know who to trust. My husband says "just pick the one with the least recovery time." But what if I die in five years because I chose the easy way? I’m 59. I want to see my grandkids graduate. I need someone to tell me what to do.
The data is unequivocal. For diabetic patients with multi-vessel disease and a SYNTAX score above 22, CABG confers a statistically significant survival advantage. The FREEDOM trial is not merely suggestive-it is definitive. To prioritize short-term convenience over long-term physiological integrity is not prudent medical decision-making. It is temporal myopia.
If you have diabetes and more than one blocked artery, CABG is the standard. Not a suggestion. Not a maybe. The guidelines are clear. Ask for the SYNTAX score. If your doctor doesn’t know it, get a second opinion. Your life is worth it.
I had CABG last year. Six weeks of pain. Three months of feeling like a ghost in my own body. But now? I walk 5 miles every morning. No chest tightness. No meds except the basics. I’m 64. I didn’t choose this for me-I chose it for my kids. If you’re young, strong, and want to live without fear? Go with the bypass. It’s not glamorous. But it’s real.
I’m a nurse in cardiac rehab. I’ve seen both. PCI patients come back in 6 months with the same pain. CABG patients? They’re the ones gardening, traveling, playing with grandkids. The recovery is brutal, yes. But the freedom after? Unmatched. Don’t let the quick return to work fool you. It’s not a win if you’re back in the cath lab in 18 months.
STOP LYING TO PEOPLE. Doctors push PCI because it’s faster, cheaper, and they get paid more. CABG saves lives. But hospitals don’t make money on 7-day stays. They make it on 3-hour stents. I had two stents. I’m back in the hospital now with a third. My surgeon told me I should’ve had CABG five years ago. They didn’t tell me that. They told me "it’s just a stent." I’m 52. I’m broken because they lied.
I don’t believe in "gold standards." Medicine is a business. The SYNTAX score? Useful tool. But it’s also a way to make patients feel like they’re getting a scientific answer when really, it’s still guesswork with numbers. I had a score of 35. Went with PCI. Two years later, still fine. Maybe I got lucky. Maybe the system failed me. I’m not sorry I chose the quick fix.
I JUST GOT MY SYNTAX SCORE. 29. DIABETIC. I’M SCARED. BUT I’M ALSO TIRED OF BEING TOLD WHAT TO DO. I WANT TO LIVE. NOT JUST SURVIVE. I’M GOING WITH CABG. I’M TELLING MY DOCTOR: I DON’T WANT A STENT THAT BREAKS IN 2 YEARS. I WANT A FIX THAT LASTS. I’M READY FOR THE RECOVERY. I’M READY TO BE STRONG AGAIN.
To the person who said "I’m scared"-you’re not alone. I was you. I cried for three days after my diagnosis. I called every patient forum I could find. I read every study. I asked my surgeon to explain the SYNTAX score like I was five. He did. And then I chose CABG. It’s not about being brave. It’s about being informed. You’ve already taken the hardest step: asking. Now go get that heart team. They’re out there. And they’re waiting for you.