Post‑operative Eye Inflammation: Surgeon Insight & Management Guide
Post-Operative Eye Symptoms Checker
This tool helps determine if your post-operative eye symptoms require immediate medical attention. Remember: most mild inflammation is normal, but some symptoms indicate an emergency.
Select symptoms and click "Check My Symptoms" to see if you should contact your surgeon immediately.
Key Takeaways
- Post‑operative eye inflammation is a normal, but sometimes risky, response after intra‑ocular surgery.
- Identifying the cause early-whether it’s a mild uveitis or an early sign of endophthalmitis-lets surgeons intervene quickly.
- Topical corticosteroids and NSAIDs are the backbone of treatment, but dosing depends on the type of surgery.
- Patients can lower their risk by following drop schedules, avoiding rubbing, and attending all follow‑up visits.
- Red‑flag symptoms such as sudden pain, vision loss, or heavy discharge require immediate medical attention.
What Is Post‑operative Eye Inflammation?
When a surgeon opens the eye for a procedure-cataract removal, vitrectomy, or glaucoma filtration-tiny tissues get irritated. The body answers with an inflammatory cascade that brings blood cells, fluid, and cytokines to the site. In everyday language, surgeons call this postoperative eye inflammation a controlled immune reaction that can turn harmful if it stays unchecked. Most of the time the swelling clears in a week or two, but a few patients develop persistent uveitis or, worse, an infection.
Common Triggers After Different Eye Surgeries
Not every eye operation triggers the same level of inflammation. Understanding the nuances helps surgeons pick the right prophylactic drops.
- Cataract surgery is the most common intra‑ocular procedure. The incision is tiny, yet the lens capsule release can spark a brief anterior uveitis.
- Vitrectomy removes the gel‑like vitreous and often involves longer operative times, increasing the chance of postoperative inflammation.
- Trabeculectomy creates a new drainage pathway for glaucoma. The bleb surface can become inflamed, especially if there’s postoperative leakage.
- Any intra‑ocular surgery can unintentionally introduce microbes, leading to endophthalmitis, a severe, vision‑threatening infection.
Even non‑surgical factors matter. Dry eye, allergies, or pre‑existing ocular surface disease can amplify the inflammatory response.
How Surgeons Spot Inflammation Early
In the first 24‑48hours after surgery, surgeons perform a slit‑lamp exam. They look for a few key signs:
- Cell and flare in the anterior chamber-captured quantitatively with a laser flare meter, which measures light scattering caused by protein leakage.
- Redness and conjunctival injection, especially around the incision site.
- Elevated intra‑ocular pressure, which can rise if inflammatory cells block the trabecular meshwork.
- Presence of hypopyon (pus in the anterior chamber) - a red flag for endophthalmitis.
When the flare reading spikes above 15 photons/ms, surgeons know the inflammation is more than the usual postoperative haze and may adjust treatment.
Management Strategies: Meds and Monitoring
The cornerstone of therapy is topical anti‑inflammatory drops. Below is a quick comparison of the two main classes.
| Feature | Corticosteroid eye drops | Non‑steroidal anti‑inflammatory drugs (NSAIDs) |
|---|---|---|
| Mechanism | Suppresses cytokine production and leukocyte migration | Inhibits cyclo‑oxygenase enzymes, reducing prostaglandin levels |
| Typical potency | High (e.g., prednisolone acetate 1%) | Moderate (e.g., bromfenac 0.07%) |
| Onset of action | Within hours | 12‑24hours |
| Risk of raised intra‑ocular pressure | Yes, especially with prolonged use | Rare |
| Effect on macular edema | Strongly reduces risk | Provides some protection but less than steroids |
For uncomplicated cataract cases, many surgeons start patients on a steroid taper for a week and add an NSAID for the first three days to curb pain. After vitrectomy, a more aggressive steroid regimen-often prednisolone acetate 1% four times daily-helps control posterior segment inflammation.
If a patient shows steroid‑induced pressure spikes, surgeons switch to a NSAID‑only protocol or add a topical carbonic anhydrase inhibitor.
In rare cases of infectious endophthalmitis, intravitreal antibiotics are administered promptly, and steroids are paused until the infection is under control.
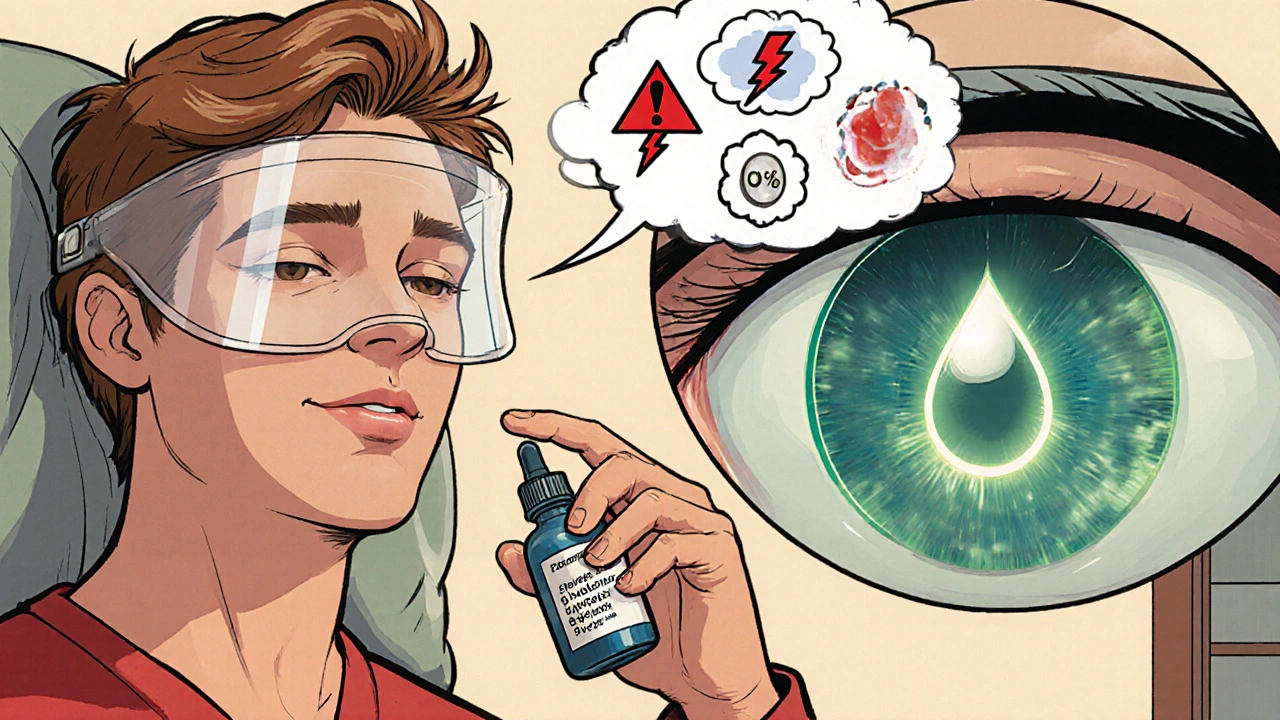
Preventive Tips for Patients
Even the best surgical technique can’t replace patient compliance. Here are practical steps patients can take:
- Start drops exactly as prescribed-missing a dose can let inflammation flare.
- Wash hands thoroughly before handling any bottle; avoid touching the tip to the eye.
- Do not rub the eye, especially in the first 48hours; mechanical trauma can increase cell leakage.
- Wear the protective shield provided by the surgeon, even if you feel fine.
- Attend every scheduled follow‑up. The laser flare meter reading can change dramatically between visits.
Patients with dry eye or allergic conjunctivitis should discuss pre‑operative eye‑drop regimens; controlling the ocular surface before surgery reduces post‑operative inflammation by up to 30% (a 2024 study from the Australian Ophthalmic Society).
When to Call Your Surgeon
Most redness and mild blur are expected. However, some symptoms signal an emergency:
- Sudden, severe eye pain that does not improve with drop use.
- Rapid loss of vision or new “floaters” that weren’t there before.
- Visible pus, heavy discharge, or a worsening red halo around the incision.
- Persistent fever or feeling generally ill after surgery.
If any of these appear, patients should contact the surgeon’s office immediately or go to the nearest emergency department. Early treatment can prevent permanent vision loss.
Looking Ahead: Emerging Strategies
Research in 2025 is exploring sustained‑release corticosteroid implants that dissolve over weeks, eliminating the need for frequent drops. Early trials show comparable control of inflammation with fewer pressure spikes. Until these become widely available, the combination of topical steroids, NSAIDs, and diligent monitoring remains the gold standard.
Frequently Asked Questions
How long does post‑operative eye inflammation usually last?
For most cataract or glaucoma surgeries, noticeable inflammation subsides within 7‑10days. More invasive procedures like vitrectomy can take 2‑4weeks, especially if the retina was involved.
Are steroid eye drops safe for everyone?
Generally yes, but patients with a history of glaucoma or steroid‑responsive intra‑ocular pressure spikes need close monitoring. Alternatives like NSAIDs or low‑potency steroids are used in those cases.
Can I use over‑the‑counter anti‑inflammatories for my eyes?
No. Oral NSAIDs don’t reach therapeutic levels in the eye and can cause systemic side effects. Only ophthalmic formulations prescribed by the surgeon should be used.
What is the role of the laser flare meter?
It quantifies protein leakage in the anterior chamber, giving an objective number to track inflammation. Values above 15 photons/ms typically trigger a change in medication.
Should I avoid wearing contact lenses after surgery?
Yes, at least until the surgeon clears you. Contacts can trap bacteria and disturb the healing incision.

Post‑operative inflammation is something every patient should keep an eye on. Even a mild uveitis can turn nasty if we don’t catch it early. Following the drop schedule exactly the way the surgeon prescribes makes a huge difference. I always remind my friends to wash their hands before touching any eye‑drop bottle.
The guide overstates the rarity of steroid‑induced pressure spikes.
Inflammation after cataract surgery usually settles within ten days, while vitrectomy may need three to four weeks. Using a laser flare meter provides an objective measure to adjust therapy promptly.
The numbers you see on a flare meter are not just random; they guide us when to ramp up steroids or add NSAIDs. A reading above fifteen photons per millisecond is a clear signal that the eye is fighting harder than expected. That’s why I always double‑check the meter at each follow‑up. It’s amazing how a simple metric can prevent a lot of trouble.
In the delicate dance of ocular healing, inflammation acts both as a messenger and a meddler, delivering the necessary signals to rebuild tissue while occasionally overstepping its bounds. Imagine the eye as a tiny city; the immune cells are the emergency responders, rushing in with cytokines and fluids to patch up the breach made by surgery. When they arrive in measured doses, they clear debris and set the stage for regeneration, but when their convoy becomes a traffic jam, vision can suffer. The surgeon’s toolbox-steroids, NSAIDs, and monitoring devices-serves as the city’s traffic controller, directing the flow and timing of the response. A corticosteroid drop works like a seasoned mayor, imposing strict regulations on leukocyte migration and cytokine production, instantly calming the uproar. NSAIDs, on the other hand, act as the diligent sanitation crew, quietly inhibiting the cyclo‑oxygenase pathways that produce swelling‑inducing prostaglandins. The synergy between the two is comparable to a well‑coordinated orchestra, each instrument knowing when to play softly and when to dominate. Yet, just as a city can be overwhelmed by a sudden storm, an eye can be besieged by infection, turning a benign uveitis into endophthalmitis within hours. The laser flare meter, that unassuming photon counter, becomes the meteorologist, warning us of an incoming squall before the clouds darken the retina. By interpreting its readings-values crossing the fifteen‑photon threshold-we can preemptively adjust medication, avoiding the cascade that leads to macular edema or pressure spikes. Moreover, patient compliance functions as the citizen’s willingness to heed evacuation orders; missing a drop is akin to ignoring a siren, and the consequences can be severe. Protective shields, proper hand hygiene, and abstaining from eye‑rubbing are the civic duties that keep the city safe during recovery. When steroids raise intra‑ocular pressure, switching to an NSAID‑only regimen is like rerouting traffic around a blocked avenue, maintaining flow while preventing a jam. In the rare event of infection, pausing steroids mirrors shutting down a noisy market to let the cleaning crew work undisturbed. Emerging sustained‑release implants promise to deliver medication continuously, much like an automated sprinkler system that waters the garden without constant human intervention. Until such technology becomes commonplace, the tried‑and‑true combination of topical steroids, NSAIDs, and vigilant monitoring remains the gold standard for preserving sight.
The poetic view of inflammation is beautiful, yet the reality hits you hard when a patient’s vision blurs unexpectedly. It’s like watching a drama unfold where the heroes are drops and the villains are rogue cytokines. I can’t help but feel a pang of helplessness when compliance falters, even though I’m merely observing the cascade.
Hey team, great rundown! If you’re feeling overwhelmed by the drop schedule, set a reminder on your phone-trust me, it saves a lot of stress. Keep those eyes clean and stay in touch with your surgeon; you’ve got this!
So you think a simple reminder will magically fix everything? Let’s not forget that the real drama happens when a patient skips the steroids and the pressure spikes like a bomb. I’d suggest a backup plan, maybe a written chart on the fridge, just in case.
Oh sure, because everyone loves juggling a slew of eye drops while pretending it’s a spa day. Thanks for the checklist, I’ll add it to my ever‑growing to‑do list that never ends.
Post‑op inflammation is common; follow the doctor’s orders and you’ll avoid most problems.
Alright folks let’s break this down step by step first you gotta understand that inflammation is not some evil force it’s actually a natural part of the healing process but when it goes overboard it can turn the whole recovery upside down so the key is balance you want enough response to clear out debris but not so much that it damages the delicate structures of the eye now the steroids are like the fire fighters they put out the flames quickly but they can leave a mess if used too long like raising the pressure inside the eye that’s why we keep a close eye on those numbers and the NSAIDs are the firefighters sidekicks they keep the fire from spreading they’re slower to act but they help prevent scarring and long term damage also don’t forget the patient’s role in this drama they need to be diligent not just slap on drops and forget about them they should keep the eye shield on protect the incision and avoid rubbing because that can re‑ignite the inflammation finally regular follow ups are the safety net the surgeon uses to catch any surprise flare ups early and adjust treatment as needed so stay vigilant keep those appointments and stick to the regimen you’ll come out on the other side with crystal clear vision
Great summary, just remember that if a patient feels overwhelmed, breaking the schedule into smaller chunks can make it easier to follow. Encourage them to keep a log and celebrate each day they stay on track.
Dear colleagues,; please note that adherence to the postoperative anti‑inflammatory regimen is paramount; a deviation may precipitate complications; consequently, I recommend implementing a systematic reminder protocol for all patients; this will ensure consistency and optimal outcomes.
Sure, but all the fancy reminders won’t help a stubborn patient who refuses to listen; the real drama is in the eye itself battling the inflammation.
lol the whole drop thing sounds like a never ending spa day right? who needs that much hassle when you could just skip it and hope for the best.
Let’s channel that energy into something positive – think of each drop as a tiny step toward clearer vision, a gift you give yourself and your loved ones who rely on your sight.
It is imperative that we prioritize domestic research and protocols over imported recommendations, as they often fail to account for our specific patient demographics and healthcare infrastructure.
Ah yes, because ignoring valuable global findings always leads to better outcomes – a truly enlightened approach.