Prilocaine for Migraine Relief: A Promising Treatment
Exploring Prilocaine as a Migraine Treatment
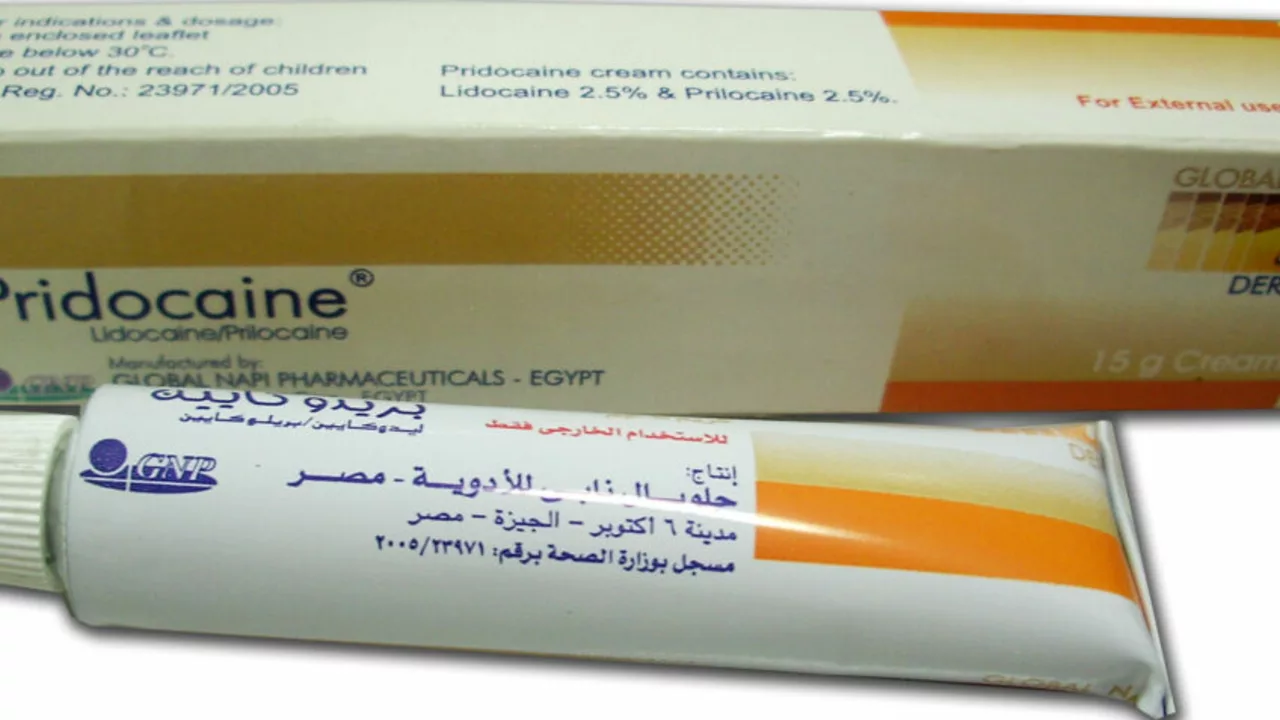
In recent years, researchers have been exploring the potential of prilocaine as a migraine treatment. Prilocaine is a local anesthetic, commonly used in dentistry and minor surgical procedures to numb the skin and relieve pain. The idea of using prilocaine for migraine relief is based on the theory that it can help in blocking the pain signals in the brain that are responsible for causing migraines. In this article, we will discuss the potential benefits of prilocaine for migraine sufferers, how it is administered, and the possible side effects that may arise from its use.
A Look at Migraine Symptoms and Causes
Migraines are a common neurological disorder characterized by severe, pulsating headaches that can last anywhere from a few hours to several days. These headaches are often accompanied by other symptoms such as nausea, vomiting, and sensitivity to light and sound. Migraine attacks can be triggered by various factors, including stress, hormonal changes, certain foods and drinks, and sleep disturbances, among others. While the exact cause of migraines is still unknown, it is believed that they result from abnormal brain activity that affects nerve signals and blood vessels in the brain.
How Prilocaine Works for Migraine Relief
Prilocaine is a local anesthetic that works by blocking the transmission of pain signals in the nerves. When administered for migraine relief, it is believed to target the trigeminal nerve, which is responsible for transmitting pain signals from the face and head to the brain. By blocking these signals, prilocaine may help to provide relief from the debilitating pain of migraines. Furthermore, its numbing effect can also help alleviate other associated migraine symptoms such as nausea and sensitivity to light and sound.
Administering Prilocaine for Migraine Treatment
Prilocaine is typically administered as an injection in a clinical setting. For migraine treatment, the injection is usually given in the forehead, temple, or the base of the skull, targeting the trigeminal nerve. The dosage and frequency of administration may vary depending on the severity and frequency of migraine attacks, as well as the patient's response to the treatment. It is important to note that prilocaine injections should only be administered by a qualified healthcare professional who is experienced in treating migraines with local anesthetics.
Potential Benefits of Prilocaine for Migraine Sufferers
Prilocaine injections have shown promising results in providing relief for migraine sufferers. In some cases, patients have reported a significant reduction in the frequency and intensity of their migraine attacks. Additionally, prilocaine may offer a faster onset of relief compared to other migraine treatments, such as oral medications, which can take some time to take effect. This rapid relief is particularly beneficial for those who experience sudden and severe migraine attacks that can be debilitating and disrupt their daily activities.
Possible Side Effects and Risks
As with any medication, there is a potential for side effects when using prilocaine for migraine relief. Some common side effects include redness, swelling, and pain at the injection site. In rare cases, more serious side effects may occur, such as allergic reactions, difficulty breathing, and changes in heart rate. It is important to discuss any concerns or potential risks with your healthcare provider before starting prilocaine injections for migraine treatment.
Conclusion: Prilocaine as a Promising Migraine Treatment
In conclusion, prilocaine injections have shown potential as a promising treatment for migraine relief. By targeting the trigeminal nerve and blocking pain signals, prilocaine may provide rapid and effective relief from migraine pain and associated symptoms. However, it is important to weigh the potential benefits against the potential risks and side effects of this treatment, and to discuss your options with a qualified healthcare professional. As research continues to explore the benefits of prilocaine for migraine sufferers, it is hoped that this treatment option may offer a much-needed solution for those who struggle with the debilitating pain of migraines.

Ah, the latest attempt to repurpose a dental anesthetic for cerebral torment, how delightfully avant‑garde. One must commend the sheer audacity of proposing pralocaine-though you spelled it "prilocaine" correctly-yet the execution reads like a hastily assembled PowerPoint. The article, while replete with citations, nevertheless suffers from a paucity of rigorous double‑blind trials, which any discerning scholar would demand. Nonetheless, kudos for venturing beyond the usual pharmacologic tropes.
Honestly, this so‑called miracle drug is just another excuse for the pharma lobby to line their pockets 🇺🇸💰. They brag about "rapid onset" as if we're all living on the edge of a migraine cliff waiting for a miracle shot. It's a classic case of over‑hyping a local anesthetic while ignoring real, evidence‑based therapies 😒. Grow up, scientists, and stop selling snake oil. 😂
From a holistic standpoint, exploring neural modulation is commendable, yet we must weigh novelty against proven efficacy. The balance between innovation and patient safety remains paramount.
Picture this: a bright burst of relief lighting up the tempestuous storm of a migraine, courtesy of a humble numbing agent-how gloriously poetic! Yet we cannot ignore the undercurrent of risk that ripples through each injection, a reminder that even the most vibrant ideas need sober scrutiny. As patriots of science, we owe it to our compatriots to demand thorough testing. Let's keep the conversation lively and grounded.
The proposition of employing prilocaine as a therapeutic modality for migraine warrants a meticulous appraisal.
First, the pharmacodynamics of prilocaine delineate its primary action as a sodium channel blocker within peripheral nerves.
Its efficacy in attenuating nociceptive transmission when administered peripherally has been well documented in dental analgesia.
However, extrapolating this peripheral mechanism to central trigeminal pathways introduces a series of physiological uncertainties.
The blood‑brain barrier imposes a formidable obstacle to the diffusion of local anesthetics of this molecular size.
Moreover, the vascular supply to the trigeminal root entry zone is uniquely regulated and may not permit uniform drug distribution.
Clinical trials that have attempted similar intraneural injections have reported variable outcomes and occasional adverse events.
The reported side effects such as hematoma, infection, and transient facial palsy underscore the procedural risks inherent to invasive techniques.
In addition, the dosage required to achieve central analgesia may exceed the safe systemic threshold for cardiac toxicity.
Prilocaine’s metabolite o‑toluidine is known to precipitate methemoglobinemia in susceptible individuals.
Consequently, any therapeutic regimen must incorporate rigorous monitoring of oxygen saturation and arterial blood gases.
From a regulatory perspective, the lack of FDA approval for this indication mandates a compassionate use protocol under investigational new drug status.
The ethical considerations surrounding experimental pain management further complicate the clinical decision‑making process.
Until robust randomized controlled trials establish a favorable risk‑benefit ratio, the routine adoption of prilocaine for migraine remains speculative.
In summary, while the concept is intellectually stimulating it must be tempered by empirical evidence and patient safety imperatives.
Hey folks, I totally get the excitement around new migraine solutions-any hope is worth a cheer. If you’re considering this option, make sure you discuss it thoroughly with a neurologist who knows the ins and outs. Supporting each other through trial and error is how we all find what truly works.
Another half‑baked idea that won’t cure migraines.
Desiree here-while I see the frustration, let’s channel that energy into demanding solid data rather than dismissing every novel approach outright. Constructive critique drives progress.
So, the “meticulous appraisal” you champion is apparently a veil for hidden agendas 😉. You’d think a drug with a simple numbing action couldn’t be part of a grand scheme, yet there’s a pattern of under‑reporting side effects that never gets highlighted. Remember, every breakthrough comes with a shadow, and sometimes the shadows are funded.
Oh brilliant, because what the world truly needs is another artisanal painkiller with a garnish of pretension. Your eloquent prose almost convinces me that we should replace all existing migraine therapies with a splatter of dental anesthetic. Bravo for the literary flourish, truly.
lol ur kinda right but also not lol i think the article could’ve used less fancy words and more real data. i mean if they had actually tested it on a decent sample size we’d know wtf’s going on. also, don’t forget to check the side effects lol.
hey i hear ya – it’s wild how we jump from fancy lingo to “lol” real quick. maybe we can all pitch in and ask the researchers for the raw numbers? that way we’d all feel included in the conversation and actually get some solid info.