Switching Between Generic Medications: What You Need to Know

Every time you pick up your prescription, you might get a different pill. Same active ingredient. Different color. Different shape. Different name on the label. If you’ve ever looked at your medicine bottle and thought, “Wait, this isn’t what I got last month,” you’re not alone. In Australia, the U.S., and most developed countries, switching between different generic manufacturers is now the norm - not the exception.
Why Do Generics Keep Changing?
Generic drugs are cheaper versions of brand-name medicines. Once a patent expires, multiple companies can make the same drug. Pharmacies and insurers pick the cheapest option available. That means your levothyroxine, warfarin, or epilepsy medication might come from Teva one month, Mylan the next, and Sandoz the month after. It’s not a mistake. It’s how the system works to save money. In the U.S., over 90% of prescriptions are filled with generics. In Australia, it’s close to 80%. And the cost difference is huge. A brand-name drug might cost $150 a month. The generic? $15. That’s why insurers push for the lowest price. But here’s the problem: not all generics are the same.What Does “Bioequivalent” Really Mean?
The FDA and TGA (Therapeutic Goods Administration) require generics to be bioequivalent to the brand-name drug. That means the amount of active ingredient in your bloodstream should be within 80% to 125% of the original. Sounds precise, right? Not quite. Imagine two different generic versions of the same drug. One delivers 80% of the brand’s concentration. The other delivers 125%. That’s a 45% difference between the two generics - even though both are “approved.” For most drugs, this doesn’t matter. But for some, it can be dangerous.When Switching Can Be Risky: Narrow Therapeutic Index Drugs
Some medications have a narrow therapeutic index (NTI). That means the difference between a dose that works and a dose that harms you is tiny. Even a small change in blood levels can cause serious problems. Three drugs fall into this high-risk category:- Levothyroxine (for hypothyroidism): A slight drop in levels can make you tired, gain weight, or feel depressed. A spike can cause heart palpitations or bone loss. Many patients report feeling awful after switching manufacturers - and their TSH levels prove it.
- Warfarin (a blood thinner): Too little, and you risk a clot. Too much, and you bleed internally. INR levels must stay in a narrow range. Studies show switching generics can cause INR spikes, even if randomized trials say otherwise. Real-world patients don’t always get lucky.
- Tacrolimus and other transplant drugs: These keep your body from rejecting a new organ. A tiny drop can trigger rejection. A tiny rise can damage your kidneys. Doctors monitor blood levels closely - but not always after a generic switch.
- Antiepileptic drugs: Patients on generic versions of phenytoin, carbamazepine, or lamotrigine report breakthrough seizures after switching. One Reddit user said: “My seizures came back after my pharmacy switched from Mylan to Teva. My neurologist checked my levels - they dropped 30%.”

What Patients Are Saying
Surveys and patient forums tell a clear story. Out of 1,247 reviews on PharmacyChecker.com:- 68% said they noticed no difference.
- 22% said the generic didn’t work as well.
- 10% said they developed new side effects.
Why Doctors Don’t Always Know
Here’s a shocking fact: 62% of doctors in a 2023 AMA survey didn’t know their patients had switched generics - until the patient complained. Why? Because pharmacies don’t notify prescribers. Insurance companies decide. Pharmacists fill the prescription. And the patient gets a different pill. Your doctor doesn’t see the manufacturer name on the bottle. They see “levothyroxine 50 mcg.” But that’s not enough. The formulation matters.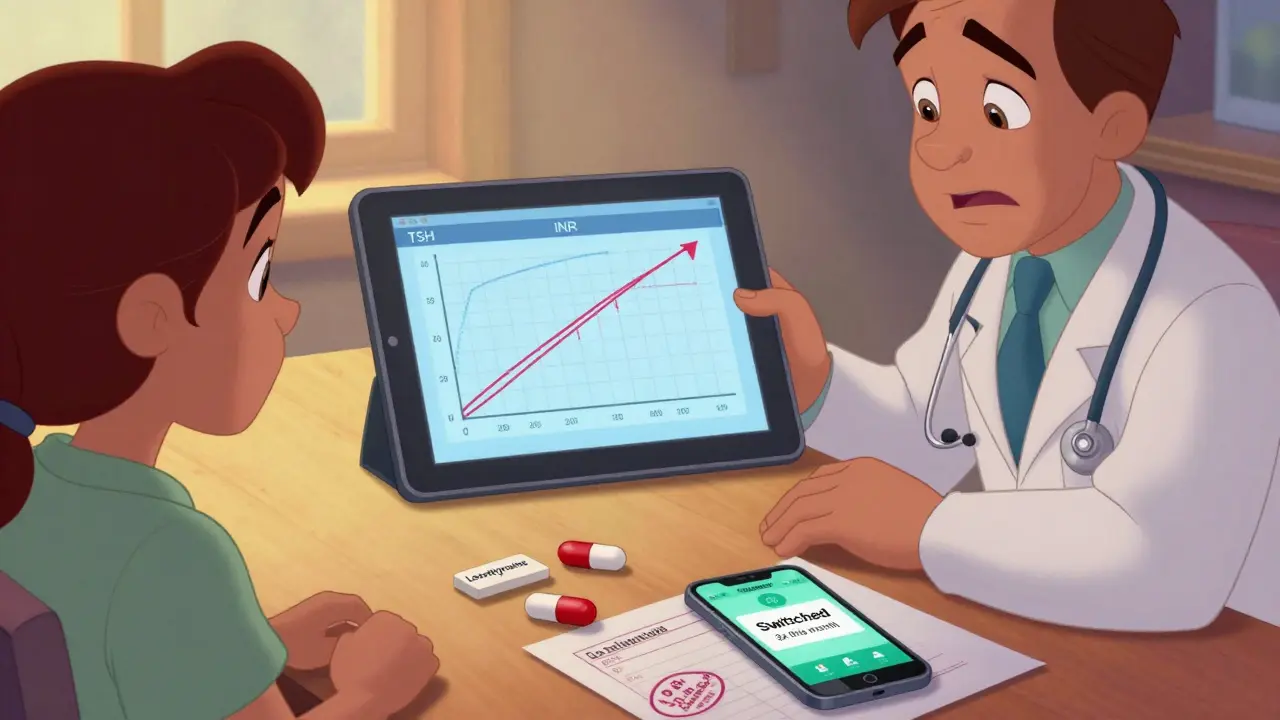
What You Can Do
You don’t have to accept random switches. Here’s how to take control:- Check your pill. Take a photo of your medication when you first get it. Note the shape, color, and imprint code (like “Teva 50” or “Mylan 25”). If it changes next refill, ask why.
- Ask your pharmacist. “Is this the same manufacturer as last time?” If they say no, ask if you can stick with one brand. Many pharmacies can special-order a specific generic.
- Request a “lock-in”. For NTI drugs, ask your doctor to write “Dispense as Written” or “Do Not Substitute” on the prescription. This legally stops the pharmacy from switching without your doctor’s approval.
- Monitor your symptoms. If you feel different after a switch - tired, anxious, dizzy, or having seizures - get your levels checked. Don’t wait. For levothyroxine, get a TSH test 4-6 weeks after a switch. For warfarin, get an INR test within 1-2 weeks.
- Use a pill tracker app. Apps like Medisafe or MyTherapy let you log which manufacturer you’re on. If you feel off, you can show your doctor the pattern.
What’s Being Done About It
Regulators are waking up. In June 2024, Medsafe (New Zealand’s drug regulator) issued new guidance: “Avoid switching between different brands of levothyroxine where possible.” The FDA is running pilot programs to track formulation changes in generics. The Association for Accessible Medicines is working on standardizing pill appearances to reduce confusion. But until those changes roll out, the burden is on you.Bottom Line
Generic drugs save billions. That’s good. But assuming all generics are identical is dangerous - especially for critical medications. If you’re on a drug with a narrow therapeutic index, switching manufacturers isn’t harmless. It’s a medical event. You have the right to know what you’re taking. You have the right to ask for consistency. Don’t let cost savings come at the cost of your health.If your medication works - and you feel fine - keep using it. But if you notice a change in how you feel after a switch, speak up. Your doctor needs to know. And you deserve to be in control of your treatment.

This is absolute madness. I switched from Mylan to Teva levothyroxine last year and spent six weeks feeling like a zombie-weight gain, brain fog, heart racing. My doctor acted like I was crazy until my TSH spiked to 12.5. Now I demand the same brand every time. If your pharmacy tries to switch you, say NO. Your life isn’t a cost-cutting experiment.
The systemic abstraction of pharmaceuticals into interchangeable commodities reflects a broader epistemological failure in healthcare delivery. The assumption of bioequivalence as sufficient for clinical equivalence disregards pharmacokinetic variance in subpopulations.
Pharmacokinetic variability in NTI drugs is well-documented in the literature, particularly for levothyroxine and tacrolimus. The 80–125% bioequivalence window, while statistically valid for population-level outcomes, fails to account for inter-individual sensitivity thresholds. This is not a flaw in generics per se, but in regulatory interpretation of bioequivalence as therapeutic equivalence.
PLEASE, if you're on thyroid meds or seizure meds-write 'DO NOT SUBSTITUTE' on your prescription! I did this after my INR went wild with a warfarin switch. My pharmacist now calls me first. Also, take a photo of your pill every time. I keep a folder on my phone. It saved me. Seriously. Do it.
This is a critical issue that requires coordinated action between patients, pharmacists, and prescribers. The lack of transparency regarding manufacturer changes undermines informed consent. Would we accept similar variability in insulin dosing or chemotherapy regimens? The ethical implications warrant regulatory reform.
STOP LETTING PHARMACIES SWITCH YOUR MEDS! I was fine for years on one brand-then BAM, new pill, seizures came back. I cried in the pharmacy. I screamed at my doctor. I won. You can too. You’re not being dramatic-you’re being smart.
so like... i just found out my levothyroxine changed again? and i felt like i was drowning in slow motion for two weeks?? i thought it was stress or my period or... idk. i never thought it was the pill. i mean, it’s the same name right?? but now i’m like... maybe i should’ve been keeping track??
Hey, if you're on one of these high-risk meds, you're not alone. I’ve been there. I started using Medisafe to track every switch-and I finally got my doctor to write 'Dispense as Written.' It’s not hard. It’s not selfish. It’s basic self-care. You deserve stability. Don’t let anyone make you feel crazy for asking.
I’ve been on generic lisinopril for 8 years. Five different makers. Never had an issue. Maybe it’s just not a big deal for everyone?
Back home in Nigeria, we don't even get generics consistently. Sometimes we get expired stuff or fake pills. I’m glad you have this problem. At least you have choices.
Regulatory agencies must mandate manufacturer labeling on all prescription containers. Transparency is not optional. The current system violates the principle of patient autonomy. A standardized, non-negotiable disclosure protocol is ethically imperative.
Everyone’s freaking out over generics. Meanwhile, the brand-name drugs are 10x more expensive and just as likely to have batch variations. You’re all just mad because you’re not getting free stuff.
Thank you for sharing this. I’ve been silently suffering with my thyroid meds for months and thought I was just ‘getting older.’ I’m going to my doctor tomorrow with my pill photos and a printout of this article. I’m done being a passive patient.
In Japan, pharmacists are required to inform patients of generic switches and provide a printed comparison sheet. It’s simple, respectful, and effective. Why can’t we adopt something similar here? It’s not about cost-it’s about dignity.