Phosphate Binder: What You Need to Know
Phosphate binders are medicines taken with meals to lower the amount of phosphate your body absorbs. Doctors usually prescribe them for people with chronic kidney disease or on dialysis, because failing kidneys can't remove phosphate well. High phosphate raises the risk of bone disease and heart problems, so controlling it matters.
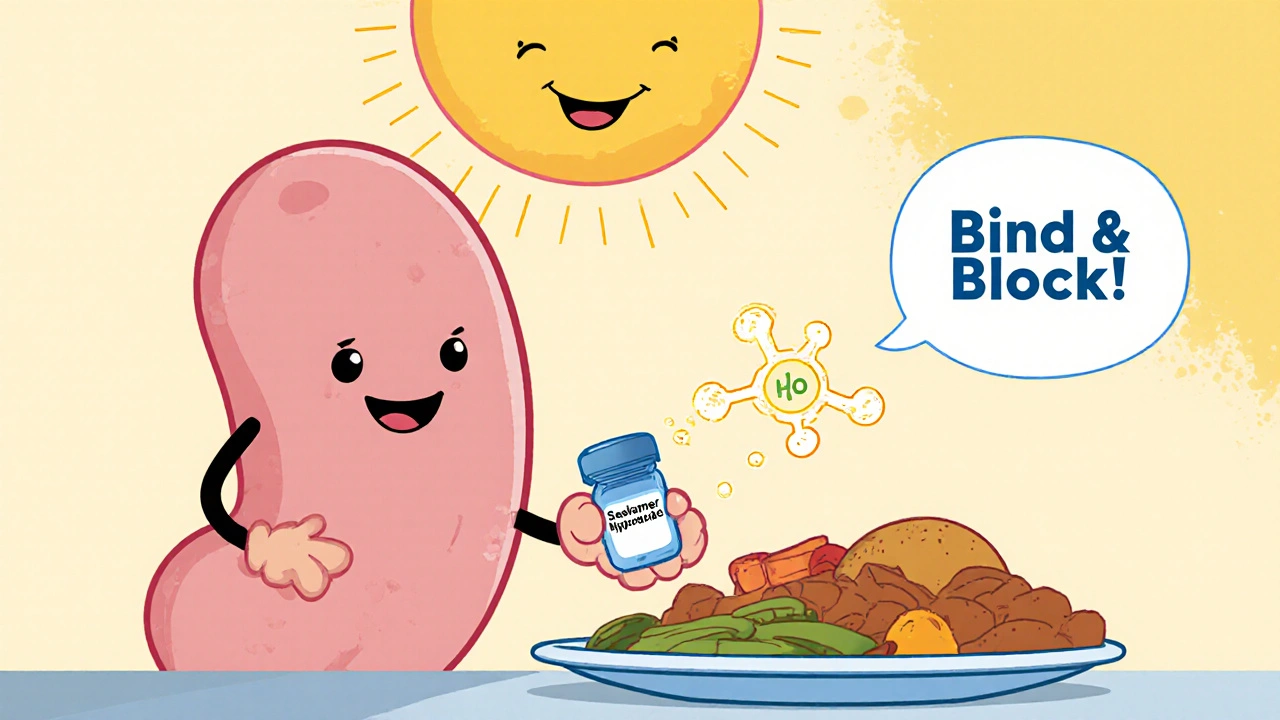
How phosphate binders work
These drugs sit in your gut and grab phosphate from food, forming a compound that passes out in stool. That reduces blood phosphate levels without changing your kidney function. Common options include calcium-based binders (like calcium carbonate), non-calcium binders (sevelamer, lanthanum), and iron-based binders (ferric citrate, sucroferric oxyhydroxide). Each works a little differently and has pros and cons.
Calcium binders are cheap and effective but can raise blood calcium, which may cause vascular calcification in some people. Sevelamer doesn’t add calcium and can lower LDL cholesterol. Lanthanum is effective but often comes as larger tablets. Iron-based binders can help iron levels but need monitoring to avoid iron overload.
Practical tips for using phosphate binders
Take them with meals or right before eating—timing matters. If you forget and eat, taking a binder later won't bind the phosphate already absorbed. Swallow tablets whole unless your pharmacist says otherwise. Spread doses across meals if your doctor prescribes multiple pills each day.
Watch for side effects: constipation is common, especially with calcium and lanthanum. Sevelamer can cause bloating and gas. Report severe stomach pain, black stools, or signs of high calcium like nausea and confusion. Your care team will check blood phosphate, calcium, and PTH regularly to adjust treatment.
Think about interactions. Phosphate binders can reduce the absorption of other drugs—carry a list and ask when to space medications. For example, bisphosphonates, levothyroxine, and some antibiotics may need timing adjustments. Ask your pharmacist for a simple schedule to avoid problems.
Diet still helps. Cutting down on processed foods, cola drinks, and high-phosphate additives lowers the pill burden. Choose fresh foods, read labels for “phosphate” or “phosphoric” ingredients, and talk to a renal dietitian for meal plans that fit your lifestyle and dialysis schedule.
Choosing the right binder depends on blood tests, other medical issues, pill burden, side effects, and cost. If you struggle with side effects or tablet size, tell your doctor—switching to a different binder often helps. Never stop binders suddenly without medical advice; phosphate can rise quickly.
Quick fact: phosphate binders are a practical tool for people with kidney disease. Use them with meals, check labs regularly, watch for side effects, and combine treatment with dietary changes. Your healthcare team will tailor the choice to your needs—ask questions so you understand why a specific binder fits you.
Ask about bloodwork frequency and which targets to aim for — target phosphate often under 5.5 mg/dL (varies by lab), and doctors may adjust based on calcium and PTH. Check coverage and cheaper generic options if cost is an issue. If you have swallowing problems, ask about powder or liquid forms. Keep a current meds list handy.