The Long-Term Effects of Carbidopa-Levodopa Treatment on Parkinson's Disease Progression
Understanding Parkinson's Disease and Carbidopa-Levodopa Treatment
Parkinson's disease is a progressive neurological disorder that affects movement, speech, and cognitive functions. The main symptoms of Parkinson's disease include tremors, stiffness, and slow movement. Although there is no cure for Parkinson's, there are several treatments available to help manage the symptoms and improve the quality of life for those living with the disease. One of the most common and effective treatments is the combination of carbidopa and levodopa, which helps to increase the levels of dopamine in the brain.
In this article, we'll explore the long-term effects of carbidopa-levodopa treatment on the progression of Parkinson's disease. We'll discuss how the treatment works, the benefits it provides, and some of the potential side effects and complications associated with long-term use. By understanding these aspects, we can better appreciate the role of carbidopa-levodopa in managing Parkinson's symptoms and improving the lives of those affected by the disease.
How Carbidopa-Levodopa Works to Manage Parkinson's Symptoms
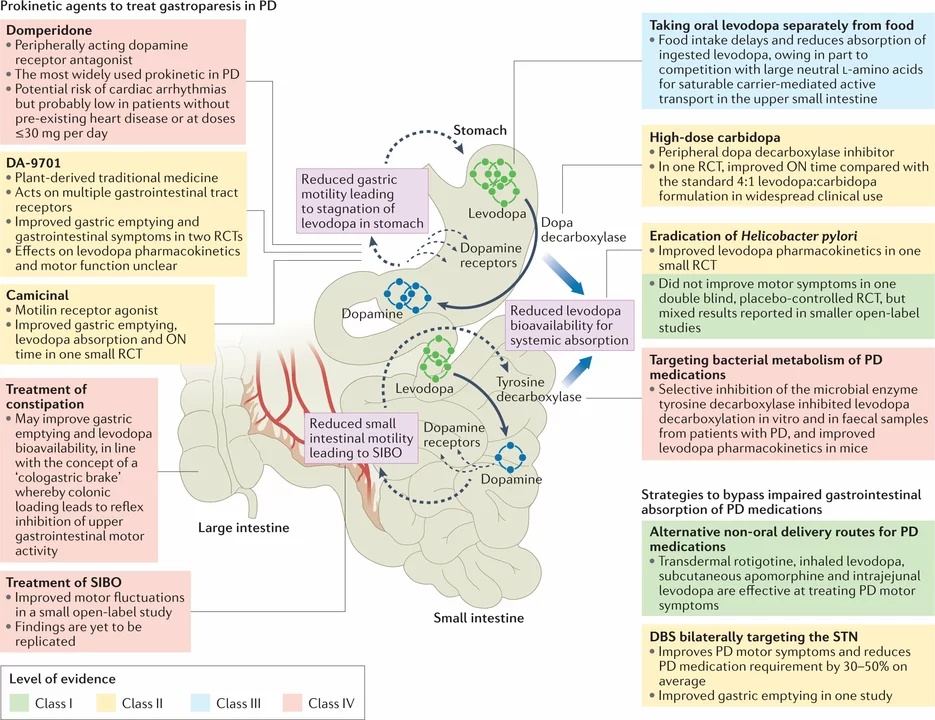
Carbidopa-levodopa is a combination medication that works by increasing the amount of dopamine in the brain, which helps to improve the motor symptoms of Parkinson's disease. Levodopa is a precursor to dopamine, and it can cross the blood-brain barrier to be converted into dopamine within the brain. However, when taken alone, a significant amount of levodopa is broken down in the body before it reaches the brain. This is where carbidopa comes in – it helps to prevent the breakdown of levodopa, allowing more of it to reach the brain and be converted into dopamine.
By increasing the levels of dopamine in the brain, carbidopa-levodopa can help to alleviate the motor symptoms associated with Parkinson's disease, such as tremors, rigidity, and bradykinesia (slow movement). This can greatly improve the quality of life for those living with Parkinson's and allow them to maintain their independence for longer.
The Benefits of Long-Term Carbidopa-Levodopa Treatment
Long-term carbidopa-levodopa treatment has been shown to provide several benefits for those living with Parkinson's disease. The most significant benefit is the improvement in motor symptoms, which can help patients maintain their mobility and independence for a longer period of time. This can also lead to a reduction in the need for assistance with daily activities and a decreased risk of falls and injuries.
Additionally, carbidopa-levodopa treatment has been associated with improvements in non-motor symptoms, such as mood, cognition, and sleep quality. These improvements can contribute to an overall better quality of life for those living with Parkinson's disease.
Side Effects and Complications of Long-Term Treatment
While carbidopa-levodopa can provide significant benefits for those living with Parkinson's disease, there are some potential side effects and complications associated with long-term use. One of the most common side effects is the development of motor fluctuations, which can cause symptoms to vary throughout the day. These fluctuations can include periods of increased mobility and reduced symptoms, known as "on" times, as well as periods of decreased mobility and increased symptoms, known as "off" times.
Another potential complication of long-term carbidopa-levodopa treatment is the development of dyskinesias, which are involuntary movements that can be mild or severe. Dyskinesias can be managed by adjusting the dosage of carbidopa-levodopa or by adding other medications to the treatment regimen.
Other side effects of long-term carbidopa-levodopa treatment can include nausea, dizziness, and low blood pressure. It's important for patients and their healthcare providers to closely monitor and manage these side effects to ensure the best possible outcomes.
Strategies for Optimizing Long-Term Treatment Outcomes
There are several strategies that can be used to optimize the long-term outcomes of carbidopa-levodopa treatment for Parkinson's disease. One important strategy is the careful titration of the medication dosage, which can help to minimize side effects and maximize symptom control. Additionally, the use of extended-release formulations of carbidopa-levodopa can help to provide more consistent symptom relief throughout the day.
Another important strategy is the use of adjunctive medications to manage specific symptoms or side effects. For example, medications such as dopamine agonists, monoamine oxidase inhibitors, and catechol-O-methyltransferase inhibitors can be added to the treatment regimen to help manage motor fluctuations and dyskinesias.
Finally, lifestyle modifications, such as regular exercise, a healthy diet, and proper sleep hygiene, can also play a crucial role in optimizing the long-term outcomes of carbidopa-levodopa treatment for Parkinson's disease.
The Future of Carbidopa-Levodopa Treatment and Parkinson's Disease Research
As research continues to advance, there is hope for the development of new therapies to improve the long-term outcomes for those living with Parkinson's disease. One area of research is focused on finding ways to slow down or halt the progression of the disease, which could potentially reduce the need for long-term carbidopa-levodopa treatment. Additionally, studies are underway to explore the potential of gene therapy, stem cell therapy, and other novel approaches to treat Parkinson's disease.
In the meantime, carbidopa-levodopa remains an essential treatment option for managing the symptoms of Parkinson's disease and improving the quality of life for those affected. By understanding the long-term effects of carbidopa-levodopa treatment and working closely with healthcare providers to optimize treatment strategies, patients can experience the best possible outcomes and maintain their independence for as long as possible.

Long‑term levodopa feels like a blessing and a curse rolled into one.
The relentless march of Parkinson’s is a cruel reminder that we are nothing but mortals trapped in a decaying shell.
Carbidopa‑levodopa, hailed as a miracle, is often presented as the sole savior in glossy pamphlets.
Yet beneath the veneer of motor relief lies a dark undercurrent of dependency and volatility.
Each dose rewires the brain’s dopamine pathways, forcing them into a precarious dance that can tip at any moment.
Patients celebrate the restored ability to sip a coffee without tremors, only to watch the “off” periods creep in like an unwelcome tide.
The on‑off fluctuations become a cruel joke, as the drug that once granted freedom now dictates the rhythm of daily life.
Dyskinesias emerge, those involuntary writhing movements that mock any sense of dignity.
You might think an extended‑release formulation would smooth the peaks, but it often just prolongs the agony.
The non‑motor side effects-sleep disturbances, mood swings, and nausea-sneak into the night and linger through the day.
Doctors prescribe adjunct therapies, hoping to patch the cracks, but each addition adds another layer of complexity.
The moral hazard is clear: we trade short‑term symptom control for a long‑term cascade of complications.
Meanwhile, research chases elusive disease‑modifying agents, promising a future that constantly recedes.
Until then, patients are left balancing on a razor‑thin line between relief and ruin.
The ethical dilemma for clinicians is palpable; do we prioritize immediate quality of life or warn of the hidden price?
In the end, we must confront the uncomfortable truth that the very medicine meant to calm the storm can also stir it anew.
The combination of carbidopa and levodopa remains the cornerstone of symptomatic management, as it effectively augments cerebral dopamine levels, thereby mitigating motor deficits in Parkinson’s disease.
When we consider the neurochemical balance, we observe that external supplementation merely postpones the inevitable neuronal attrition, prompting reflection on the transient nature of pharmacological solace.
That’s a thoughtful point; while the meds can’t halt degeneration, they do buy precious time for patients to enjoy moments that would otherwise be lost.
Sticking to a consistent dosing schedule and incorporating low‑impact exercise can really smooth out the on‑off swings and keep daily life more predictable.
Sure, but if you keep ignoring the dyskinesia warnings and just push higher doses, you’re basically signing a death‑warrant for quality of life – it’s not “just a bit more” but a slippery slope.
Don’t forget to talk with your neurologist about extended‑release options; they often help flatten the peaks and valleys – it’s worth a chat! 😊
Honestly, all this hype around “optimizing” dosing feels like reinventing the wheel – just take the meds and call it a day.
While I respect the enthusiasm, it’s crucial to set clear limits on dosage escalation to avoid severe side effects.
Look, Jeff, you’re right about limits, but many patients still get pushed beyond safe thresholds because the clinical guidelines are vague; a tighter protocol would help.
Oh great, another “miracle” pill that works until it doesn’t – guess we’re all just waiting for the next shiny thing while the disease keeps marching on.
Seriously, Alex, the sarcasm is noted, but sarcasm won’t fix the motor fluctuations – solid research and patient‑centered care will.