Type 2 Diabetes Remission: How Weight Loss Can Lead to Medication De-escalation
For millions living with type 2 diabetes, the idea of getting off medication isn’t just a dream-it’s becoming a realistic goal. But it’s not about cutting pills because you feel better. It’s about changing your body in a way that lets your pancreas and liver function again. That’s what type 2 diabetes remission really means.
What Does Remission Actually Mean?
Remission isn’t a cure. It’s not magic. It doesn’t mean your diabetes disappeared forever. It means your blood sugar has stayed below 6.5% HbA1c for at least three months-without taking any diabetes meds. That’s the official definition set in 2021 by the American Diabetes Association, the European Association for the Study of Diabetes, and other major health groups. Before this, doctors used different standards. Some counted anyone with normal sugar levels as being in remission-even if they were still on metformin or insulin. Now, if you’re on meds, you’re not in remission. Period. Why does this matter? Because it changes how you think about your diagnosis. Instead of seeing diabetes as a life sentence of pills and needles, you start seeing it as a condition you can actively reverse. That shift in mindset helps people stick with hard changes. And those changes? They’re mostly about weight.Weight Loss Is the Main Driver
The most powerful tool for triggering remission? Losing weight. Not a little. Not “maybe lose 5 pounds.” We’re talking about losing at least 10 kilograms (about 22 pounds), and often more. The DiRECT trial showed that 46% of people who lost 10kg or more went into remission after one year. That’s nearly half. And in the ARMMS-T2D study, 37.5% of people who had metabolic surgery-usually because they were severely overweight-were in remission after three years. It’s not about being thin. It’s about reducing fat around your liver and pancreas. When that fat builds up, it messes with how your body makes and uses insulin. Lose the fat, and those organs start working again. You don’t need to be a bodybuilder. You just need to get below your personal fat threshold. Total diet replacement programs-where people replace meals with nutritionally balanced shakes for a few months-have worked well in trials. So have low-calorie diets under medical supervision. The key? It’s not the diet name. It’s the calorie deficit. And the consistency.Who Has the Best Chance?
Not everyone has the same shot at remission. Your odds go up if:- You’ve had type 2 diabetes for less than five years
- Your HbA1c was below 8% when you started your weight loss journey
- You’re not on insulin
- You’re younger than 60

Medication De-escalation Isn’t the Goal-Remission Is
Some doctors talk about “reducing meds” as a win. But the goal isn’t to take fewer pills. The goal is to take zero pills-and stay there. If you’re still on metformin, even if your HbA1c is 5.8%, you’re not in remission. That’s a common misunderstanding. That’s why the 2021 consensus is so clear: remission requires stopping all glucose-lowering drugs. Not just cutting back. Stopping. And then maintaining normal blood sugar for at least three months. Some experts, like Dr. Michael Nauck, suggest we might need a second category: “partial remission” where people are off some meds but still on others. But right now, the official standard doesn’t include that. If you’re still taking anything to lower your blood sugar, you’re managing diabetes-not reversing it.It Doesn’t Last Forever-Unless You Keep Working
Here’s the hard truth: remission can fade. The DiRECT trial showed that after two years, only 36% of people who initially reached remission were still there. Why? Weight came back. Lifestyle slipped. The body, once trained to store fat, doesn’t forget. That’s why remission isn’t a finish line. It’s a new starting point. You still need to eat well. You still need to move. You still need to see your doctor yearly for HbA1c checks and to monitor for complications. Even if your sugar is perfect, your heart risk doesn’t vanish overnight. You’re not cured. You’re in control. NHS Scotland’s Right Decisions platform puts it plainly: “Remission stops diabetes in its tracks-but only if you keep doing the work.”What About Other Treatments?
Weight loss isn’t the only path. Bariatric surgery, like gastric bypass, can trigger remission in up to 40% of cases. But surgery isn’t for everyone. It’s expensive. It’s risky. And it’s not always covered by insurance. Newer medications like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro) help people lose weight-and some patients do go into remission while on them. But here’s the catch: if you’re still taking those drugs, you don’t meet the official remission criteria. The consensus is clear: meds disqualify you. That doesn’t mean those drugs aren’t valuable. They are. For many, they’re life-changing. But if your goal is true remission-no meds, no compromises-you need to focus on diet, movement, and sustained weight loss.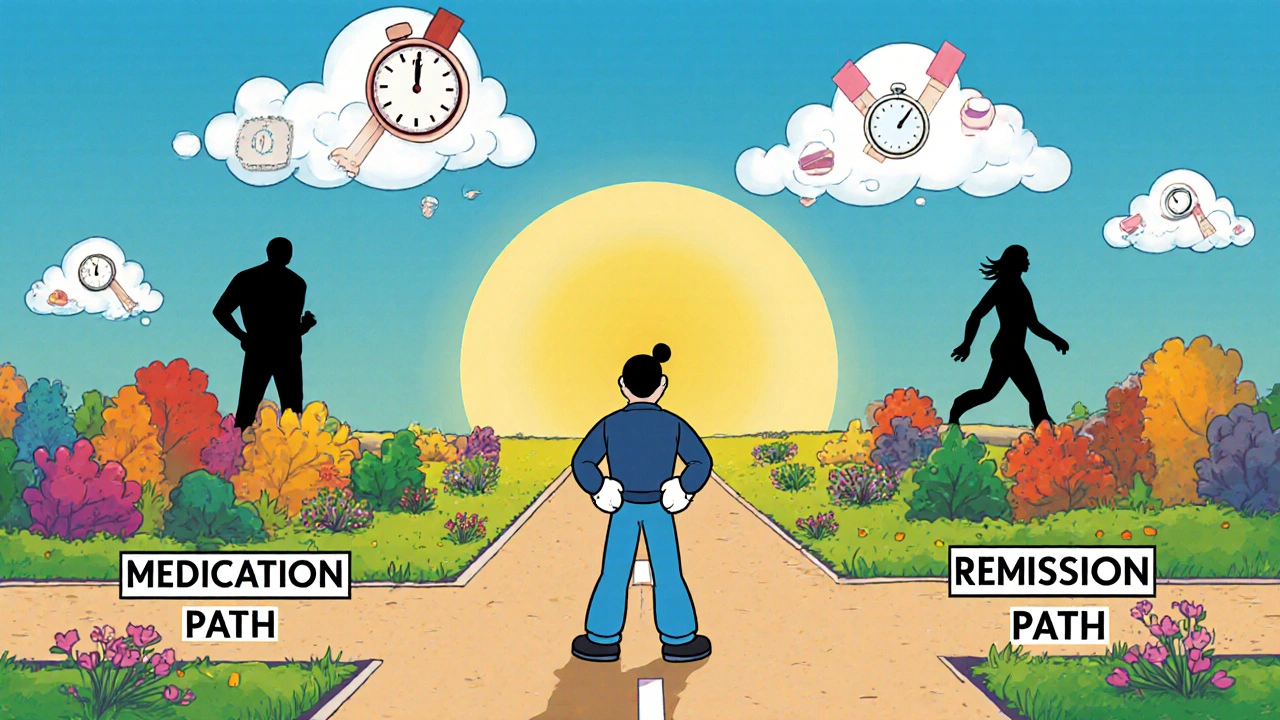
What Happens If You Relapse?
If your HbA1c creeps back up above 6.5%, it doesn’t mean you failed. It means your body is asking for help again. That’s normal. Many people go in and out of remission multiple times. Each time you return to healthy habits, you delay complications. You lower your risk of nerve damage, kidney disease, heart attack, and stroke. Think of it like this: every year you spend in remission is a year your body isn’t being damaged by high sugar. That matters. Even if you eventually need meds again, you’ve bought yourself time. And time is the most valuable thing you can have with diabetes.How to Start
If you’re thinking about aiming for remission, here’s how to begin:- Get your HbA1c tested. If it’s above 8%, focus on lowering it first with your doctor’s help.
- Work with a dietitian or diabetes educator. Don’t try to guess your way through a low-calorie plan. You need structure.
- Set a realistic weight goal. Losing 10kg is a strong target. If you’re heavier, aim for 15% of your body weight.
- Track your progress with regular HbA1c tests-not just daily glucose checks. HbA1c tells the real story.
- Don’t stop meds without your doctor’s approval. Even if you feel great, sudden changes can be dangerous.
- Prepare for the long haul. Remission isn’t a 3-month sprint. It’s a lifestyle you live forever.
The Bigger Picture
Type 2 diabetes affects 1 in 10 adults in the U.S. and rising. If even a fraction of those people can reach remission, it changes everything. Fewer heart attacks. Lower healthcare costs. Less suffering. But we can’t do it with pills alone. We need to change how we eat, move, and think about our bodies. The science is clear. The tools exist. The only thing missing? The will to stick with it.Can type 2 diabetes be cured?
No, type 2 diabetes cannot be cured. Remission means blood sugar levels are normal without medication for at least three months-but the underlying tendency for insulin resistance remains. If weight is regained or lifestyle changes stop, blood sugar can rise again. Remission is a state of control, not a permanent fix.
Do I need to stop all my diabetes meds to be in remission?
Yes. According to the 2021 international consensus, remission is only recognized if you’ve been off all glucose-lowering medications-including metformin, GLP-1 agonists, and insulin-for at least three months while maintaining HbA1c below 6.5%. If you’re still taking any of these drugs, even if your sugar is normal, you’re managing diabetes, not in remission.
How long does remission last?
There’s no set timeline. Some people stay in remission for years. Others see blood sugar rise again within months. The DiRECT trial showed 36% remained in remission after two years. Long-term data is still limited, but weight maintenance is the biggest predictor. The more weight you keep off, the longer remission lasts.
Can I get remission if I’m on insulin?
It’s possible but rare. Insulin use usually means the pancreas has lost most of its ability to make insulin. Weight loss can help, but most people who’ve been on insulin for years still need it. Remission is much more common in those who use only oral meds or no meds at all. Still, some have reversed insulin dependence with aggressive weight loss-always under medical supervision.
What if my HbA1c is normal but I’m still on metformin?
You’re not in remission. You’re successfully managing your diabetes. Metformin helps lower blood sugar, so even if your HbA1c is 5.7%, the medication is doing the work. True remission requires stopping all glucose-lowering drugs. Your doctor may consider reducing or stopping metformin if you’ve lost weight and your sugar stays normal-but that’s a separate decision from remission.
Should I try for remission if I’m happy on my current meds?
That’s a personal choice. If your meds are working, your sugar is stable, and you’re not struggling with side effects, there’s no medical need to change. But if you want to reduce your long-term health risks, avoid complications, or feel more in control of your body, aiming for remission through weight loss can be powerful. Talk to your doctor about your goals-they can help you decide if it’s right for you.
Does remission lower my risk of heart disease?
Evidence suggests it does. High blood sugar damages blood vessels over time. When you achieve remission, you reduce that damage. Studies show people in remission have lower rates of heart attack, stroke, and kidney disease compared to those with ongoing high sugar-even if they’re on meds. But we don’t yet have long-term data proving remission cuts mortality. Still, every year with normal sugar is a year your heart is protected.
Can I get remission without losing a lot of weight?
Unlikely. The strongest evidence shows that losing at least 10kg is needed for most people. Some individuals with very short diabetes duration and low starting weight may see improvement with less-but this is uncommon. The science consistently links fat loss around the liver and pancreas to improved insulin function. Without significant weight loss, remission is rare.

Losing 10kg and walking away from meds? Sounds too good to be true but I’ve seen it happen. My uncle did it. No surgery. No magic pills. Just stopped eating like a college kid and moved more. Now he’s off everything and feels 20 years younger. Still eats pizza once a month though. Life’s not perfect but it’s better.
THIS. 🙌 I was on metformin for 4 years. Lost 28 lbs. Stopped meds. HbA1c at 5.6% for 8 months now. It’s not about being thin-it’s about giving your pancreas a break. I cried the day my doctor said I was in remission. Not because I was ‘fixed’-but because I finally felt like I had control. You’re not broken. You’re just overloaded. And you can reset. 💪❤️
In India, we call this 'reverse diabetes'-but the science is solid. Fat around liver = insulin resistance. Lose that fat = pancreas wakes up. I’ve seen patients go from HbA1c 9.8% to 5.9% in 6 months with 1200 kcal/day meal replacements. Not easy. Not quick. But possible. And the best part? No more finger pricks at 3am. You trade pills for purpose. Worth it.
Wait, so you’re telling me… if I just stop eating, I can stop taking meds? No way. This is just another fad. People gain it all back. And what about the 60% who don’t make it? You’re selling hope like it’s a supplement. Also, metformin is literally the most studied drug in history. Why throw it out? And don’t get me started on ‘total diet replacement’-that’s just starvation with a fancy name.
I want to say this gently: if you’re reading this and thinking ‘I can’t do this’-you’re not alone. I was there. I thought remission meant I had to be perfect. But it doesn’t. It just means showing up. Some days you eat salad. Some days you eat fries. Both are okay if you keep moving forward. Your body isn’t your enemy. It’s trying to survive. Help it.
remission my ass. i lost 15kg and still had to take metformin. turns out my body just hates me. also who even uses hbac1c? sounds like a typo. anyway i think this whole thing is a big pharma scam to sell more shakes.
Y’all need to stop acting like this is only for people who can afford dietitians and meal replacements. My cousin did this on a budget: beans, eggs, spinach, walking after dinner. No shakes. No fancy apps. Just consistency. She’s been off meds for 18 months. It’s not about money. It’s about making your health a priority. Even if it’s one step at a time.
Let’s be honest: this is just a glorified weight loss article. The real issue? Society’s obsession with ‘fixing’ people instead of accepting them. Diabetes isn’t a moral failing. It’s a biological reality. And now you’re making people feel guilty for needing meds? That’s not science. That’s shame wrapped in a white coat.
The epigenetic burden of chronic hyperglycemia is not erased by weight loss alone. While metabolic reprogramming occurs via reduced ectopic lipid deposition, the underlying insulin resistance phenotype persists at the cellular level. Remission, therefore, represents a transient homeostatic equilibrium rather than a true phenotypic reversal. Longitudinal biomonitoring remains imperative to mitigate latent risk.
I did it. Took me 14 months. Still have cravings. Still stress-eat sometimes. But I’m off everything. And I finally stopped hating my reflection. 🌱
Bro, I lost 22kg with just walking and cutting soda. No shakes. No dietitian. Just stopped drinking sugar water. My HbA1c dropped from 8.2 to 5.4. My mom says I’m cured. I say I’m awake. If you’re reading this and thinking ‘I can’t’, you’re already halfway there. Just start. One day. One meal. One step.
This is dangerously misleading. You’re implying that people who remain on metformin are somehow ‘failing’. That’s not just inaccurate-it’s unethical. Millions of people live full, healthy lives on medication. To frame remission as the only valid outcome is to stigmatize those who need ongoing care. This isn’t empowerment. It’s elitism dressed as science.