Urinary Retention from Medications: How Anticholinergics Can Stop You from Urinating

Urinary Retention Risk Calculator
How This Calculator Works
Based on the latest medical research, this tool helps you assess your risk of urinary retention from anticholinergic medications. Enter your details to see your personalized risk level and recommendations.
Imagine sitting on the toilet for 20 minutes, straining, feeling the urge-but nothing comes out. Then it hits you: you haven’t peed in over 12 hours. No fever, no injury, no infection. Just a pill you started last week for an overactive bladder. This isn’t rare. It’s a known, preventable side effect of common medications-and it can land you in the ER with a catheter. Anticholinergic drugs are designed to calm an overactive bladder. But what they actually do is block a key chemical in your body-acetylcholine-that tells your bladder muscle to contract. Without that signal, your bladder can’t empty. The result? Urinary retention. And for men over 65 with even mild prostate enlargement, this isn’t just uncomfortable-it’s dangerous. According to the American Urological Association, up to 10% of all urinary retention cases are caused by medications. And anticholinergics are the top culprits.
How Anticholinergics Break Your Bladder’s Natural System
Your bladder doesn’t just fill up and burst. It’s a finely tuned system. When it’s full, nerves send a signal. Acetylcholine is released. It binds to M3 receptors on the bladder wall. The muscle contracts. The sphincter relaxes. You pee. Anticholinergics block those M3 receptors. They don’t just reduce urgency-they stop the contraction entirely. The bladder fills, but can’t push out. Residual urine builds up. Over time, this stretches the bladder, weakens the muscle, and increases infection risk. It’s not just about feeling full. Acute urinary retention means you can’t pee at all. Chronic retention means you’re always leaving behind more than 100mL after going. Both require medical intervention.Which Medications Are the Biggest Risks?
Not all anticholinergics are created equal. Some are more likely to cause retention than others.- Oxybutynin (Ditropan): Highest risk. Used for overactive bladder. Odds of retention in men with BPH: 3.2 times higher than placebo.
- Tolterodine (Detrol): Moderate risk. Still 2.1 times more likely to cause retention than oxybutynin in men with prostate issues.
- Solifenacin (Vesicare): Moderate risk. 31-fold selectivity for M3 receptors, but still causes retention in 1.2-1.8% of users.
- Trospium (Sanctura): Moderate-high risk. Less brain penetration, but still blocks bladder receptors.
- Darifenacin (Enablex): More selective for M3, but still carries risk in vulnerable patients.
Who’s Most at Risk?
You’re not equally vulnerable just because you’re on these meds. Risk spikes dramatically if you:- Are male and over 65
- Have benign prostatic hyperplasia (BPH) or enlarged prostate
- Take multiple anticholinergics (e.g., for depression, allergies, or Parkinson’s)
- Are on opioids, diuretics, or alpha-adrenergic agonists
- Have dementia or cognitive impairment

Real Stories, Real Consequences
On Drugs.com, a 68-year-old man named JohnM72 wrote: “After two weeks of oxybutynin 5mg, I couldn’t pee at all. Had to get catheterized. My urologist said this happens in 1 out of 50 men my age with even mild prostate issues.” On Reddit’s r/urology, 127 posts since 2020 describe similar emergencies. One user, 71, ended up in the ER after taking tolterodine. Another, 73, had to be catheterized twice in six months because his doctor didn’t check his post-void residual. But not all stories are negative. CathyR on HealthUnlocked said: “My urologist checks my residual every month. I’ve been on solifenacin for 18 months without issues. We caught my residual creeping up to 150mL and cut my dose. That’s how you do it.” The difference? Monitoring.What Doctors Should Do (But Often Don’t)
The guidelines are clear. The American Urological Association (2022) says:- Always measure post-void residual (PVR) before starting anticholinergics in men.
- Stop the drug if PVR exceeds 150mL.
- Check PVR weekly for the first month, then quarterly.
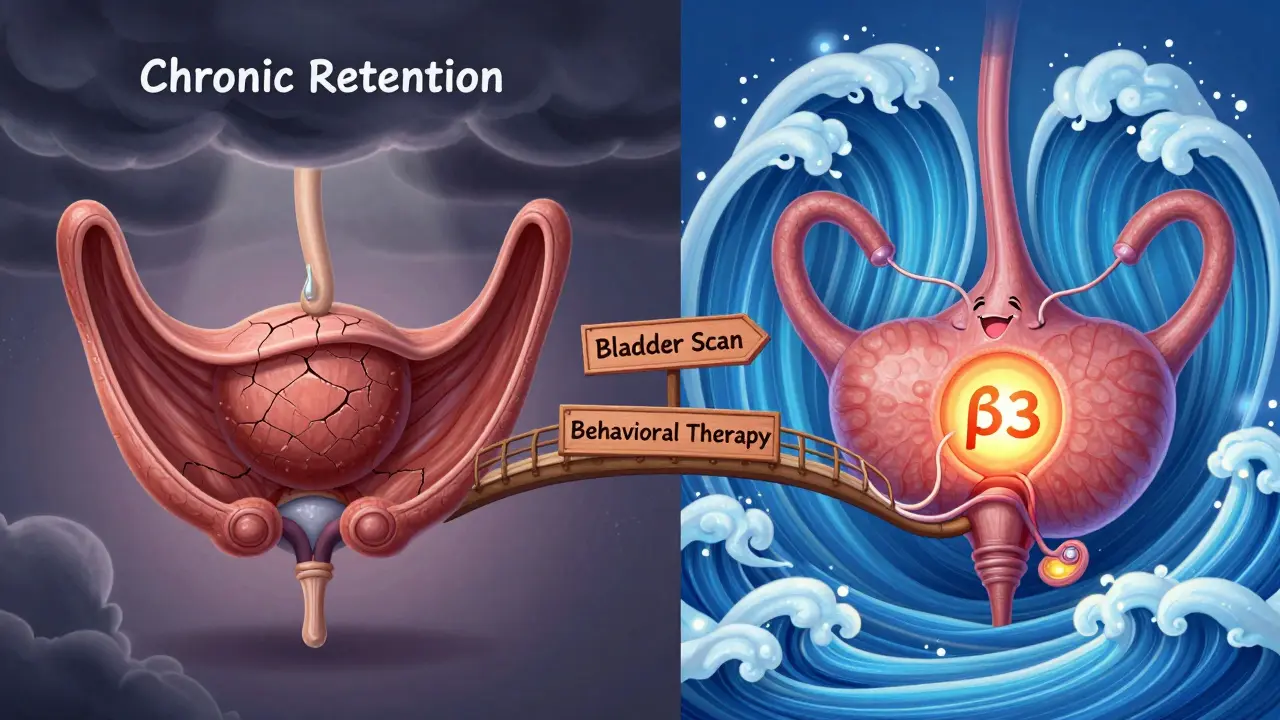
Alternatives That Don’t Risk Retention
There are safer options.- Mirabegron (Myrbetriq): Works by relaxing the bladder muscle through β3 receptors-not acetylcholine. Retention risk: 0.3%. Used in 44% of OAB prescriptions in 2022, up from 12% in 2015.
- OnabotulinumtoxinA (Botox): Injected directly into the bladder. Retention risk: 0.5%. Requires a specialist, but no systemic side effects.
- Peripheral Neuromodulation: Tiny device implanted near the tailbone to stimulate nerves. No drugs. No retention risk.
- Behavioral therapy: Bladder training, timed voiding, pelvic floor exercises. Effective for mild cases.
What You Can Do Right Now
If you’re on an anticholinergic for overactive bladder:- Ask your doctor: “What’s my post-void residual?” If they don’t know, ask for a bladder scan.
- If you’re male and over 65, and have prostate issues-ask if you really need this drug.
- Watch for these warning signs: weak stream, straining, feeling like you didn’t empty, dribbling after peeing, needing to go again 10 minutes later.
- If you can’t pee for 12 hours-go to urgent care. Don’t wait.
- Ask about switching to mirabegron or behavioral therapy.
The Bigger Picture
This isn’t just about one drug class. It’s about how we treat aging bodies. We’ve been prescribing anticholinergics for decades like they’re harmless. But the data shows they’re risky-especially for men with prostate issues. The U.S. spends $417 million a year treating drug-induced urinary retention. That’s emergency visits, catheters, hospital stays. New tools are emerging. The Anticholinergic Risk Calculator (ARC), launched in 2023, uses age, prostate size, baseline PVR, and other meds to predict individual risk with 89% accuracy. Genetic testing for CHRM3 receptor variants may soon identify who’s most vulnerable. But the simplest fix? Check the residual. Before you start. After you start. Regularly.What’s Changing in 2025?
The American Urological Association’s 2025 draft guidelines are expected to recommend no anticholinergics at all for men with prostate volume over 30mL. That’s about half the male population over 65. Mirabegron and Botox are now first-line for men. Anticholinergics? They’ve been pushed to third-line-only if nothing else works. And in Europe, the EMA now mandates contraindications on all anticholinergic labels for anyone with a history of retention. This isn’t a debate anymore. It’s a shift in practice.Can anticholinergic medications cause permanent bladder damage?
Yes, if urinary retention is chronic and untreated. When the bladder is stretched too often or for too long, the muscle can become permanently weak. This leads to chronic urinary retention, increased risk of UTIs, kidney damage, and even bladder stones. Early detection and stopping the medication can prevent this. But if you’ve been holding urine for weeks or months, damage may be irreversible.
Is urinary retention from meds more common in men or women?
Far more common in men-especially those over 65 with enlarged prostates. Women have a lower baseline risk because they don’t have prostate obstruction. Studies show men are 2-3 times more likely to experience retention from anticholinergics. A 2022 survey found 12.3% of men on these drugs had retention severe enough to need catheterization, compared to 5.1% of women.
What should I do if I can’t pee after starting a new medication?
If you haven’t urinated in 12 hours or more, go to an urgent care center or ER. Do not wait. Acute urinary retention is a medical emergency. You’ll likely need a catheter to drain your bladder. Bring your medication list. The provider will check your post-void residual and likely discontinue the anticholinergic. Don’t assume it’s just a temporary issue-it can be life-threatening if untreated.
Are there any anticholinergic drugs that are safer for the bladder?
Some have lower risk, but none are risk-free. Darifenacin and solifenacin are more selective for M3 receptors and carry slightly lower retention rates than oxybutynin. Trospium has less brain penetration, which may reduce overall side effects. But if you have an enlarged prostate or are over 65, even these carry meaningful risk. The safest approach is to avoid them entirely unless no other option exists-and only with regular bladder scans.
Can I take anticholinergics if I have a small prostate?
Even a small prostate increases risk. Prostate size isn’t the only factor-age, nerve sensitivity, and other medications matter too. A 2020 VA study found that 3.2% of all acute retention cases in men over 65 were caused by anticholinergics, regardless of prostate size. If you’re over 65, it’s safer to assume you’re at risk. Ask for a bladder scan before starting, and consider mirabegron instead.

Wait, so you're telling me Big Pharma is secretly using anticholinergics to keep old men stuck on the toilet so they can’t leave the house and start conspiracy theories? 😏 I’ve been saying this for years - they don’t want you mobile, they want you docile. Catheters = control. And don’t even get me started on how the FDA’s black box warning was buried under 17 pages of fine print. They’re not warning you - they’re warning the lawyers. I’ve got a spreadsheet on this. Want to see it?
One is reminded of the ancient Indian medical texts, which spoke of the body as a vessel of balance - where the flow of urine mirrors the flow of prana. To obstruct this natural rhythm with pharmacological force is not merely to treat a symptom, but to disrupt the harmony of the organism. The modern mind seeks control through chemical intervention, yet fails to perceive that the body’s wisdom predates the pill. Perhaps the true remedy lies not in replacing one agent with another, but in restoring the conditions under which the body may heal itself - through diet, stillness, and awareness.
Post-void residual measurement is the only clinically validated metric in this entire discussion. The lack of standardized PVR protocols across primary care is a systemic failure of urological triage. Oxybutynin’s M3 antagonism is well-characterized, but the real issue is the absence of baseline urodynamics. Without cystometry or ultrasound quantification, prescribing is speculative. And yes - mirabegron has a better safety profile, but its beta-3 agonism induces vasodilation in susceptible populations. Risk-benefit analysis is not binary. It’s a multivariate regression model with age, prostate volume, CYP2D6 genotype, and concomitant med use as predictors. You’re not ‘just’ taking a pill. You’re participating in a pharmacokinetic cascade.
i think this is so true… but also… maybe we are all just too quick to take pills? i mean, i had a friend who took oxybutynin for like 3 weeks and then couldnt pee… and he was like ‘oh well’… like… did he even think about drinking less coffee? or doing pelvic floor stretches? i think we forget that our bodies arent machines to be fixed with chemicals… they’re alive… and sometimes… they just need time… and quiet… and maybe less sugar
Let’s be clear: anyone over 65 taking an anticholinergic without a baseline PVR is either negligent or reckless. This isn’t ‘side effect’ territory - it’s malpractice waiting to happen. And for the love of God, stop calling it ‘overactive bladder’ like it’s a lifestyle choice. It’s a physiological dysfunction. If your doctor can’t or won’t measure residual volume, find a new one. You’re not ‘being difficult’ - you’re preventing a catheterization, a UTI, and possibly kidney failure. This isn’t advice. It’s a survival protocol.
YOU THINK THIS IS BAD? WAIT TILL YOU FIND OUT THE REAL REASON THEY KEEP PUSHING ANTICHOLINERGICS. THE FDA IS OWNED BY PHARMA. THE UROLOGISTS GET BONUSES FOR PRESCRIBING THEM. THE BLADDER SCANNERS ARE TOO EXPENSIVE FOR CLINICS TO BUY - SO THEY IGNORE THE RISK. AND THE PATIENTS? THEY’RE JUST NUMBERS IN A DATABASE. DID YOU KNOW OXYBUTYNIN IS IN THE TOP 5 DRUGS FOR GERIATRIC ADVERSE EVENTS? THEY KNOW. THEY KNOW. AND THEY STILL SELL IT. THIS ISN’T A MEDICAL ISSUE - IT’S A CRIME. AND YOU’RE ALL JUST SITTING THERE READING ABOUT IT LIKE IT’S A NEWS ARTICLE. GET UP. DO SOMETHING. OR NEXT TIME, IT’LL BE YOU IN THE ER WITH A CATHETER.
How utterly pedestrian. You’ve reduced a profound physiological phenomenon to a checklist of drugs and scans. The real tragedy isn’t urinary retention - it’s the collapse of medical intuition. We’ve replaced the art of diagnosis with algorithmic compliance. The elderly aren’t being harmed by oxybutynin - they’re being abandoned by a system that values efficiency over empathy. And let’s not pretend mirabegron is some noble alternative. It’s just the next branded placebo with a prettier label. True healing requires listening. Not scanning. Not dosing. Not checking boxes. Just… listening.
Actually, the real problem is that this whole post assumes everyone wants to pee normally. What if you don’t? What if the body’s slowing down is a feature, not a bug? Maybe holding it in is nature’s way of forcing stillness. Maybe we’re the ones who are broken - obsessed with constant output, constant productivity, constant voiding. The bladder isn’t malfunctioning. We are.