Vaccines and Medications: Timing With Immunosuppressants

Getting vaccinated while on immunosuppressants isn’t just about when you schedule the shot-it’s about whether it works at all. If you’re taking medication for rheumatoid arthritis, lupus, cancer, or an organ transplant, your immune system is already working under heavy restrictions. A vaccine given at the wrong time might not trigger any protection. And if you wait too long, you could be exposed to preventable diseases like flu, shingles, or pneumonia with no defense.
Why Timing Matters More Than You Think
Most people think vaccines work the same for everyone. They don’t. For someone on immunosuppressants, the immune system’s ability to respond is reduced. Studies show that up to 50% of patients on certain drugs like rituximab or mycophenolate don’t develop protective antibodies after standard vaccine doses. That’s not a failure of the vaccine-it’s a failure of timing. The goal isn’t just to get the shot. It’s to get it when your body has the best shot at building immunity. That means coordinating with your meds. If you’re on a drug that wipes out B-cells, like rituximab, waiting too long after your last dose can mean your immune system is still too weak to respond-even months later. On the flip side, getting vaccinated right before starting a new drug might mean the medication shuts down the response before it even starts.When to Get Vaccinated Before Starting Immunosuppressants
The safest window is before you even start the medication. Most guidelines agree: get all necessary vaccines at least 14 days before beginning immunosuppressant therapy. Some experts, like those at the CDC and Memorial Sloan Kettering, recommend 2 to 4 weeks. Why the range? It depends on the drug and your condition. For example:- If you’re starting methotrexate for arthritis, aim for 2 weeks before your first dose.
- If you’re preparing for chemotherapy, get your vaccines 3 to 4 weeks before your first cycle.
- If you’re on rituximab and haven’t started yet, get all non-live vaccines at least 4 weeks prior.
What Happens After You’ve Already Started the Meds?
If you’re already on immunosuppressants, timing gets trickier. You can’t just stop your meds for a vaccine-your condition might flare. But you also can’t ignore the risk of infection. Here’s how major guidelines break it down by drug class:Methotrexate
The American College of Rheumatology (ACR) recommends pausing methotrexate for two weeks after your flu shot-if your disease is under control. That’s one of the few cases where a short hold actually improves vaccine response. In one trial, patients who skipped their methotrexate dose for two weeks after vaccination had significantly higher antibody levels than those who kept taking it.Rituximab and Other B-Cell Depleters
This is where things get complicated. Rituximab wipes out B-cells, the very cells that make antibodies. Once you’ve had it, your body can’t respond to vaccines for months. The CDC and ASH say wait 3 to 6 months after your last dose before getting vaccinated. But the ACR says 6 months for all vaccines except flu. Meanwhile, IDSA’s 2025 draft guidelines say 3 to 6 months, but only if your B-cell count is below 50 cells/μL. Real-world problem? A 2023 report from Massachusetts General Hospital found 18% of patients on rituximab got shingles during their 6-month waiting period. That’s preventable illness because timing was too rigid.Biologics (TNF Inhibitors, Abatacept, etc.)
For drugs like adalimumab or etanercept, hold for one dose before vaccination, then wait 4 weeks after to restart. This gives your immune system a small window to respond. Abatacept is different-it doesn’t respond well even with timing adjustments. So if you’re on abatacept, getting vaccinated before starting it is even more critical.Chemotherapy and Immunosuppressive Pills
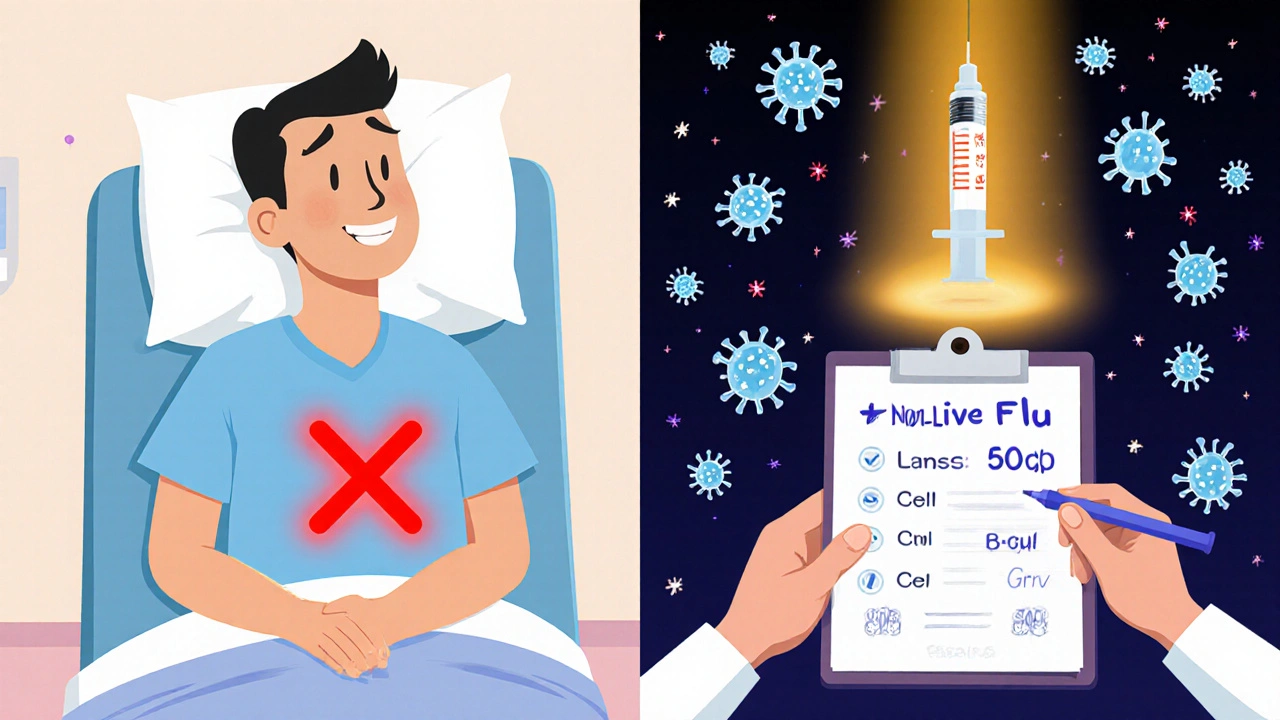
Drugs like azathioprine, mycophenolate, and cyclophosphamide don’t need to be stopped for non-live vaccines. But for live vaccines (like MMR or shingles), you need to pause them for 4 weeks before and after. IV cyclophosphamide requires stopping for one full cycle, then waiting 4 weeks after to restart.Live vs. Non-Live Vaccines: The Big Difference
Not all vaccines are the same. Live vaccines contain weakened versions of the virus. For someone with a normal immune system, that’s fine. For someone on immunosuppressants, it can be dangerous.- Live vaccines to avoid: MMR, varicella (chickenpox), nasal flu vaccine, yellow fever, BCG.
- Safe non-live vaccines: Flu shot (injected), pneumococcal, hepatitis B, HPV, tetanus, COVID-19 mRNA vaccines.
IVIG Therapy: A Special Case
If you’re getting intravenous immunoglobulin (IVIG), your body is flooded with antibodies from donors. That means your immune system doesn’t need to make its own-and vaccines won’t work as well. Here’s the catch: IVIG can block vaccine response for months. The ACR guidelines say:- 300-400 mg/kg dose → wait 8 months before live vaccines
- 1 g/kg dose → wait 10 months
- 2 g/kg dose → wait 11 months
What About the Flu Shot? It’s Still Worth It
Even if you’re on immunosuppressants, the flu shot saves lives. Studies show it reduces hospitalizations by up to 40% in this group. The problem? Many patients don’t get it because they’re afraid it won’t work. Here’s the truth: It might not work perfectly. But even partial protection matters. One study found that patients on methotrexate who paused their dose for two weeks after the flu shot had 27% higher antibody levels. That’s not 100%-but it’s enough to lower your risk of severe illness.Real Problems, Real Stories
A patient on Reddit shared: “I waited six months after rituximab for the shingles vaccine. Got shingles three weeks before my appointment. My rheumatologist said it was unavoidable.” Another said: “My oncologist timed my flu shot three weeks before chemo. I haven’t had the flu in three years-even with low white blood cells.” These aren’t outliers. They’re examples of what happens when timing is ignored vs. when it’s handled right.
The Future: Personalized Timing
Fixed time windows are fading. Experts now agree: one-size-fits-all doesn’t work. Your immune system is unique. Your drug dose, your disease, your age, your genetics-all matter. New research is shifting toward immune reconstitution monitoring. Instead of waiting 6 months after rituximab, doctors are checking your B-cell count. If it’s above 50 cells/μL, it’s safe to vaccinate. This approach is being tested in the NIH-funded VAXIMMUNE study, which is tracking 2,500 patients through 2024. Even tech companies are stepping in. Epic Systems announced a new EHR module in May 2024 that will auto-calculate safe vaccine windows based on your meds and local disease rates. It’s scheduled to roll out in 2025.1.What You Can Do Right Now
You don’t need to wait for perfect systems. Here’s your action plan:- Make a list of every medication you’re on-including doses and last administration date.
- Know which vaccines you need: flu, pneumococcal, hepatitis B, HPV, shingles (non-live), and COVID-19.
- Ask your doctor: “Is this vaccine safe with my current meds? When’s the best time to get it?”
- If you’re starting a new immunosuppressant, schedule vaccines before the first dose.
- If you’re already on meds, ask about B-cell counts or T-cell tests to guide timing.
- Don’t skip the flu shot. Even if it’s not perfect, it’s better than nothing.
Common Mistakes to Avoid
- Waiting until you’re sick to get vaccinated. Too late.
- Assuming all vaccines work the same. They don’t.
- Stopping meds without consulting your doctor. Flares can be dangerous.
- Ignoring live vaccine risks. They can cause illness in immunosuppressed people.
- Not tracking your last drug dose. Timing is useless if you don’t know when you last took it.
Final Thought: It’s Not Just About Vaccines
This isn’t just about shots. It’s about living well with a chronic condition. Vaccines are one tool in a bigger toolkit: diet, sleep, avoiding crowds during outbreaks, washing hands, and knowing when to call your doctor. But if you’re on immunosuppressants, vaccines are your first line of defense. The science is clear: timing saves lives. The challenge? Getting the system to match the science. Until then, be your own advocate. Ask the questions. Track your meds. Push for the right window. Your immune system is counting on it.Can I get the COVID-19 vaccine while on immunosuppressants?
Yes, and you should. mRNA vaccines like Pfizer and Moderna are non-live and safe. The CDC recommends getting them at least 14 days before starting immunosuppressants. If you’re already on meds, get them anyway-boosters are especially important. Studies show even partial response reduces hospitalization risk by over 50%.
Should I stop my methotrexate before the flu shot?
If your arthritis is well-controlled, yes. Hold methotrexate for two weeks after your flu shot. This boosts antibody response by up to 27%, according to clinical trials. Don’t stop it without talking to your rheumatologist-only pause it after the shot, not before.
How long after rituximab should I wait for a shingles vaccine?
Wait at least 6 months after your last rituximab dose. The ACR and CDC recommend this for non-influenza vaccines. Some experts now suggest checking your B-cell count-if it’s above 50 cells/μL, vaccination may be safe earlier. But never assume. Always test and confirm with your doctor.
Is it safe to get vaccines while on IVIG?
It depends on the dose and timing. High-dose IVIG (1-2 g/kg) can block vaccine response for 8-11 months. For live vaccines, wait the full time. For non-live vaccines, wait at least 4 weeks after IVIG. After vaccination, hold IVIG for another 4 weeks. Always coordinate with your specialist.
What if I missed the window before starting immunosuppressants?
It’s not ideal, but it’s not hopeless. Get vaccinated as soon as possible after starting. Some vaccines still work, especially if you’re on low-dose or intermittent therapy. Ask your doctor about checking antibody levels after vaccination. Boosters are often recommended for immunosuppressed patients.
Do I need to avoid people after getting a vaccine?
No, not after non-live vaccines. You can’t shed the virus from shots like flu or COVID-19 mRNA vaccines. But if you get a live vaccine (which is rare on immunosuppressants), you may need to avoid close contact with severely immunocompromised people for a short time. Always ask your doctor.
Can I get a booster if I’m on immunosuppressants?
Yes, and you should. The CDC recommends extra doses for immunosuppressed patients. For COVID-19, that means a primary series of 3 doses, followed by annual boosters. For flu, get it every year. Boosters help compensate for weaker initial responses.

Ugh, another wall of text. Can we just get a flowchart? I’m on methotrexate and I just want to know if I can get the flu shot tomorrow or if I need to schedule a therapy session with my doctor first.
While the article is comprehensive, it lacks clarity on the practical logistics: How does one actually coordinate with multiple specialists-rheumatologist, oncologist, pharmacist-when each has a different recommendation? The guidelines are not harmonized, and patients are left navigating bureaucratic contradictions.
So let me get this straight: if you’re rich enough to afford rituximab, you get to wait six months to get a vaccine. If you’re poor and on Medicaid, you get shingles and a bill for ER care. Brilliant public health policy.
I’ve been on mycophenolate for six years now, and I’ve gotten every vaccine under the sun-flu, pneumo, shingles, even the COVID boosters. I didn’t pause anything. My doctor said it’s fine. I’ve never had a serious infection. So maybe all this timing stuff is just overkill? Or maybe I’m just lucky? Either way, I’m not going to stop my meds just because some study says so.
Wow. Someone actually took the time to compile this. Must’ve been a grad student with too much free time and no social life. Next up: a 20-page PDF on how to breathe properly while on steroids.
This is exactly the kind of information that saves lives. I’m a nurse who works with transplant patients, and I’ve seen too many people skip vaccines because they were scared or confused. Thank you for laying this out so clearly. Please share this with your doctors. They might not know it all.
Don’t let the complexity scare you. Even if you’re not hitting the perfect window, getting *something* is better than nothing. I’m on adalimumab and got my flu shot two weeks after my dose. My titers were low, but I didn’t get sick. That’s a win. Keep showing up for your health, even if it’s imperfect.
Look, I get it. You’re scared. You’ve been told your immune system is broken. But here’s the truth: you’re not broken-you’re adapting. And science is catching up. The fact that we’re now talking about B-cell counts and immune reconstitution? That’s progress. Ten years ago, we were just guessing. Now we’re measuring. That’s huge. Don’t give up. Keep pushing for personalized care. You deserve it.
Every time someone says "timing matters," I think: who decided that? The pharmaceutical industry? The CDC? Who profits when you wait six months for a vaccine? Who profits when you get shingles? The system is designed to keep you docile, confused, and dependent. Wake up.
Interesting. So if I’m on IVIG, I can’t get a vaccine for 11 months? Cool. So I’m just supposed to wait until I catch something? Thanks for the reassurance.
Let me guess: this was written by someone who’s never had to choose between paying rent and buying a $1,200 vaccine. You talk about "personalized timing" like it’s a luxury. For most of us, it’s a myth. Your doctor doesn’t have time to check your B-cells. Your insurance won’t cover the test. And your pharmacy won’t stock the right vaccine because "it’s not standard." This isn’t medicine. It’s a privilege.
Thank you for the thorough breakdown. I’ve shared this with my patient support group. Many of them were unaware that pausing methotrexate after the flu shot could improve efficacy. This kind of clear, evidence-based guidance is rare. Please keep producing content like this-it makes a tangible difference in people’s lives.
Why are we letting bureaucrats and pharmaceutical companies dictate when we get vaccines? In America, we’re supposed to be free. Why can’t I just get the shot when I want it? This is overregulation. I’ve been on immunosuppressants for a decade. I’ve never gotten sick. I don’t need a PhD to tell me when to get a flu shot.
Everyone’s so focused on timing, but no one talks about how the meds make you feel like a zombie. I’m on 15 pills a day. I can barely remember my own name. And now I have to track vaccine windows? Who has the mental energy for this? I just want to feel normal for one day.
Just got my third COVID booster last week-on my usual dose of azathioprine. No pause. No drama. My doctor said it’s fine. I’m not worried. Vaccines are tools. Use them. Don’t overthink them. 🤝💉