Parkinson's disease — Symptoms, treatments, and everyday tips
Parkinson's disease is more than a tremor. It slowly affects movement, mood, sleep, and how you do everyday tasks. If you or someone you care about was just diagnosed, this short guide gives clear, practical steps you can use right away.
What it is: Parkinson's happens when dopamine-producing cells in the brain die off. That leads to the classic motor signs — tremor (usually at rest), slowness of movement (bradykinesia), stiffness (rigidity), and balance problems. Non-motor signs often come first or alongside motor ones: loss of smell, constipation, sleep changes, depression, and thinking problems.
Common treatments you should know
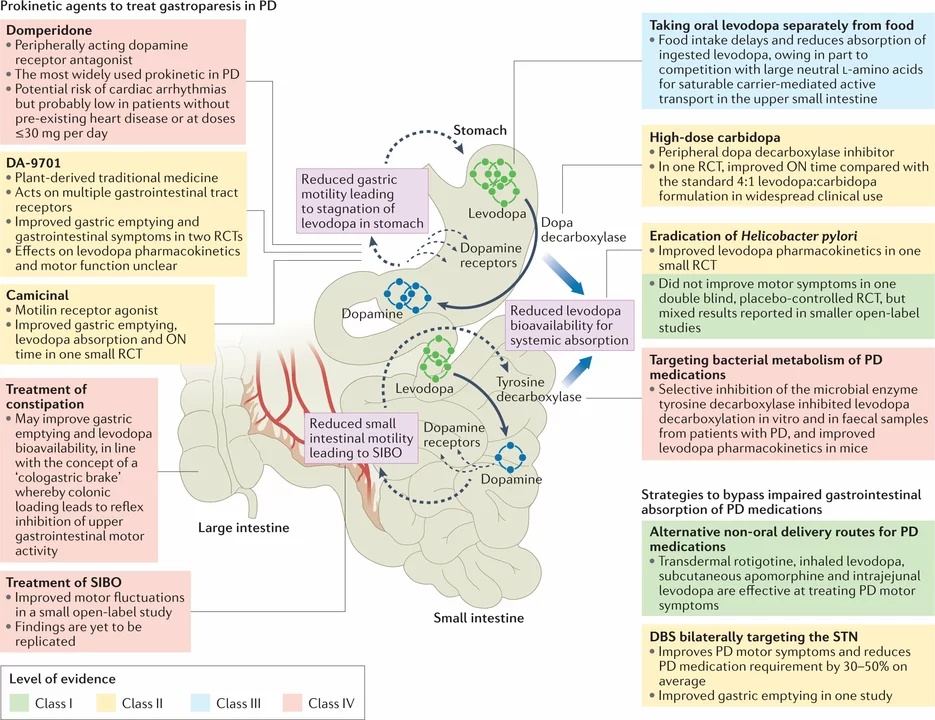
Medication is the mainstay. Levodopa is the strongest drug for improving movement; most people notice the biggest benefit from it. Dopamine agonists (for example, pramipexole) and MAO-B inhibitors are other options used alone or with levodopa. There are also COMT inhibitors and amantadine for specific situations. Each drug has trade-offs — levodopa can cause involuntary movements after years of use, while dopamine agonists can trigger impulse-control issues in some people.
For advanced cases, deep brain stimulation (DBS) can reduce symptoms and medication needs. DBS is surgery and not for everyone, but it helps many people who have strong medication fluctuations or severe side effects.
Daily management and practical tips
Small habit changes make a big difference. Keep a consistent medication schedule and use a pillbox or phone reminders. For people on levodopa, spreading protein intake away from doses can improve how well the drug is absorbed. If you notice "on-off" moments (sudden changes in mobility), tell your neurologist — adjusting dose timing or adding a drug often helps.
Exercise is powerful. Regular aerobic workouts, resistance training, dance, tai chi, or brisk walking help strength, balance, mood, and thinking. Speech therapy improves loudness and clarity; occupational therapy helps with dressing, eating, and using adaptive tools safely.
Manage non-motor problems too: treat constipation with diet and fiber, maintain good sleep habits, and get help for depression or anxiety. Watch for red flags that need urgent care — repeated falls, trouble swallowing, severe hallucinations, or sudden confusion should prompt a doctor visit.
Caregivers: simplify routines, label cupboards and drawers, remove trip hazards, and plan for medication times. Small supports — a raised toilet seat, a stable chair, or grab bars — keep daily life safer and more independent.
If you want deeper articles on specific drugs, therapies, or caregiving tips, check the Parkinson's disease tag on GoGoMeds for clear, practical reads written for real life.