Pediatric glaucoma — what every parent should know
Pediatric glaucoma is not just "adult disease in a small body." It can damage a child’s vision fast if missed. Some babies are born with it (congenital glaucoma), while others develop it later (juvenile glaucoma). Early action matters — spotting it and getting the right specialist can save sight.
How pediatric glaucoma looks
Signs can be subtle or obvious. Watch for these: an unusually large eye, cloudy cornea (hazy or whitish surface), excessive tearing, sensitivity to light, and poor visual tracking in infants. Older kids may rub their eyes a lot, complain of blurry vision, or struggle with reading. If you notice any of these, book a pediatric ophthalmology visit right away.
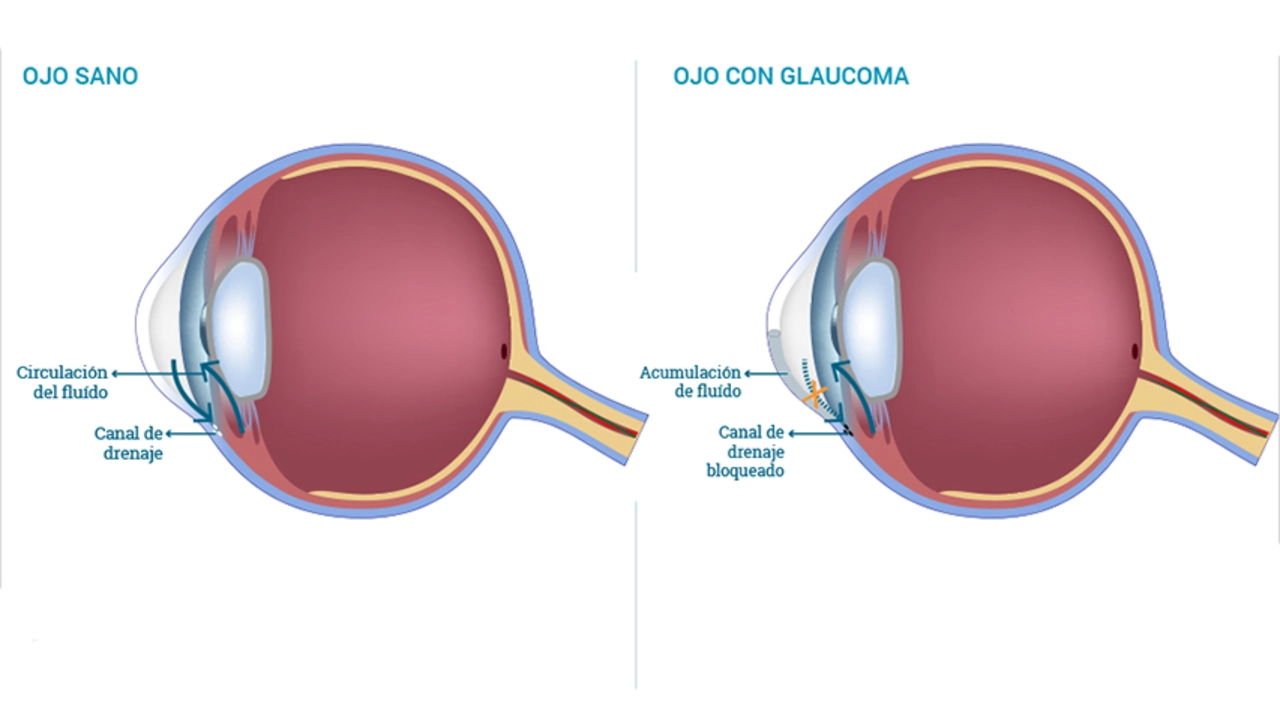
Doctors don’t rely on symptoms alone. Diagnosis usually includes measuring eye pressure (in babies this often happens under light anesthesia), checking corneal diameter, inspecting the optic nerve, and doing gonioscopy to see the drainage angle. Your child may also get photos or ultrasound of the eye. These tests help decide how aggressive treatment needs to be.
Treatment options and what parents should expect
Treatment goals are simple: lower eye pressure, protect the optic nerve, and keep vision developing normally. For many children, surgery is the first-line treatment. Common procedures include goniotomy and trabeculotomy, which open the eye’s drainage to lower pressure. If those don’t work, a trabeculectomy or a tube shunt may be used.
Topical eye drops (beta-blockers, carbonic anhydrase inhibitors, sometimes prostaglandin analogs) are used before or after surgery, or when surgery isn’t immediately possible. Drops can help but often aren’t enough alone for congenital cases. Expect repeated visits and sometimes multiple surgeries over time — pediatric glaucoma is a long-term condition, not a one-time fix.
Vision rehab is part of care. Children with uneven vision need amblyopia (lazy eye) treatment like patching or glasses. Early visual development matters; the eye needs to be monitored closely for eyesight, pressure, and corneal health.
Practical tips: get care from a pediatric ophthalmologist experienced with glaucoma, keep follow-up appointments, track medication use carefully, and ask for clear written care plans. If your family has a history of childhood glaucoma or certain genetic conditions, discuss genetic testing and earlier screening.
When in doubt, act. A quick referral and early surgery can often preserve useful vision. Pediatric glaucoma is treatable — but only when you catch it and keep up with care.